- Lectures / Webinars
- 9. Local Anesthetics, Neurolytics, and Chemodenervation for the Patient with Cerebral Palsy and Spasticity
9. Local Anesthetics, Neurolytics, and Chemodenervation for the Patient with Cerebral Palsy and Spasticity
Hot 
This section will discuss the use of local anesthetics, neurolytics and chemodenervation with BTX for the treatment of the patient with cerebral palsy and focal spasticity.
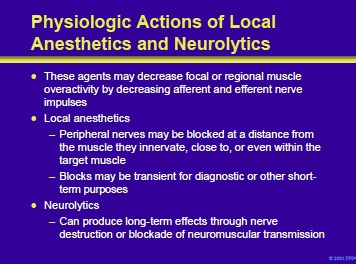
Local anesthetics and neurolytics can decrease focal or regional muscle overactivity in patients with cerebral palsy and spasticity by decreasing afferent and efferent nerve impulses. Local anesthetics (eg, lidocaine, bupivacaine, etidocaine) can reduce focal spasticity by decreasing afferent and efferent impulses in nerves supplying skeletal muscles.
Blocks may be intramuscular or perineural. Nerve blocks produced by local anesthetic agents produce short-duration effects and are predominantly used for either diagnostic purposes or for shortterm relief of focal spasticity prior to an intervention (eg, casting).
Neurolytics (eg, phenol, ethanol) produce long-term effects by destroying or severely damaging the nerve or motor points (distal motor nerve branches very close to muscle). Neurolytics produce effects that last from 2 to 5 months
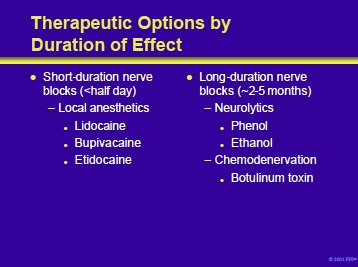
Agents that produce a neuromuscular blockade can be subdivided into short- and long-duration agents. The longduration agents can be further subdivided into those which produce dissolution of the neural tissue (eg, Phenol) and those that produce their effect by chemodenervation (eg, BTX).
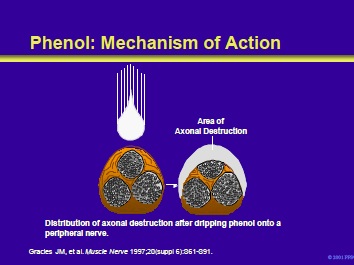
Phenol (carbolic acid) is a major oxidized metabolite of benzene. Phenol is a potent proteolytic agent. Concentrations of phenol of 5% to 7% are proteolytic and dissolve tissues on contact.
When injected immediately adjacent to a nerve, phenol in high concentrations produces a chemical neurolysis. These effects are nonselective across nerve fiber size and are most prominent on the nerve’s outer aspect. Following an injection of a neurolytic dose of phenol, local anesthetic effects are observed within 5 to 10 minutes.
After 24 hours, the long-term effects of neurolysis on the manifestations of spasticity occur. The duration of these effects may be related to the length of the nerve segment denervated. They have an average duration of 6 months but can last as long as a year.
Gracies JM, Elovic E, McGuire J, et al. Traditional pharmacological treatments for spasticity part I: local treatments. Muscle Nerve 1997;20(suppl 6):S61-S91.
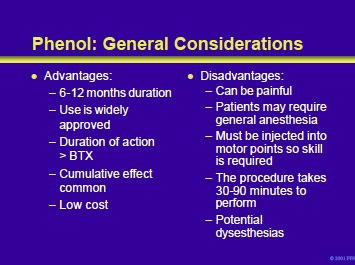
When phenol neurolysis is performed appropriately, the benefits can last for 6 to 12 months. The use of phenol for this purpose is widely approved by insurance carriers. Compared to chemodenervation with BTX, phenol neurolysis has a longer duration of action and may show a cumulative effect. In addition, phenol is inexpensive.
Neurolysis with phenol is a painful procedure. In addition, if a sensory nerve is treated, approximately 15% of adults and 5% of children will develop dysesthesias. The age difference appears to be predominant because children do not complain as often as adults. Dysesthesias are a particular problem with mixed sensory and motor nerves.
Compared to injections of BTX, children treated with this methodology often require general anesthesia. Notably, skill is required to perform neurolysis since the phenol must be injected into a motor point. Lastly, phenol injections require a significant time commitment on the part of the injector.
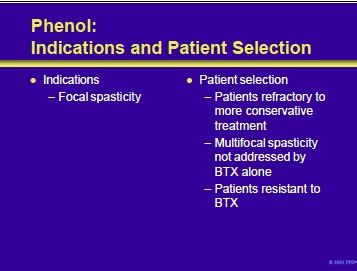
Phenol neurolysis is used to treat focal spasticity. Neurolysis with phenol can be employed in patients who are refractory to conservative measures or those too young for more aggressive approaches such as selective dorsal rhizotomy, intrathecal baclofen or orthopedic surgery.
In patients with multifocal spasticity, inadequately treated with BTX alone, the combination of phenol neurolysis and chemodenervation with BTX may provide the best overall treatment. Since one cannot develop resistance to phenol, the rare patient with true BTX resistance might also be a phenol candidate.
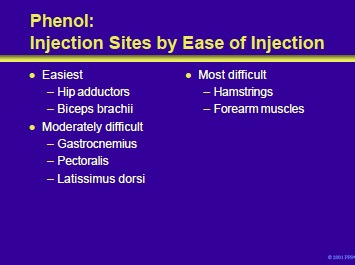
Certain nerves are easier to inject with phenol since they can be easily localized. Therefore, the best results are often observed when treating spasticity of the hip adductors (obturator nerve) or of the biceps brachii (musculocutaneous nerve).
Injection of the gastrocnemius (tibial nerve), pectoralis major (lateral and medial pectoral nerves) and latissimus dorsi (thoracodorsal nerve) are moderately difficult to inject because they may be difficult to localize. Nerves to the hamstrings and to the forearm are the most difficult.
The hamstrings provide a particular problem because the nerves can be difficult to locate in sufficient numbers to have a significant impact on the tone of those muscles.
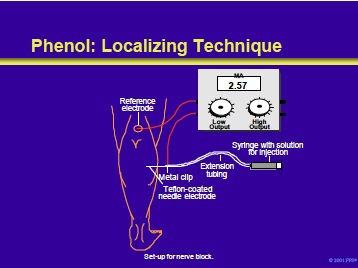
Phenol has a small diffusion capacity. Therefore, it will produce necrosis only within a range of several millimeters. This necessitates accurate localization of the injecting needle. Prior to the phenol injection, the nerve should be localized by electrode stimulation.
As mentioned previously, the localization and injection components of this procedure can be uncomfortable and general anesthesia is frequently required for children.
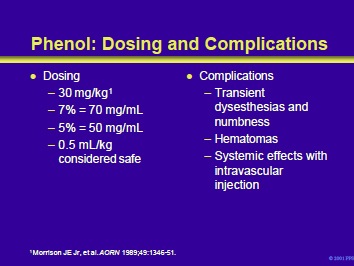
Morrison et al recommended a phenol dose of 30 mg/kg. A 5% and 7% solution of phenol contains 50 and 70 mg of phenol/mL, respectively. Therefore, when injecting a 30 kg child, the total dose should not exceed 900 mg. This can be translated into 18 mL of a 5% solution, or almost 13 mL of a 7% solution. On a volumetric basis, 0.5 mL/kg is considered to be within the limits of safety. Therefore, a 30 kg child should receive a volume of <15 mL (best supplied with a 7% solution). Injections can be repeated within days of each other.
Complications of phenol neurolysis include transient dysesthesias and numbness. The risk may be as high as 15% and is higher when mixed motor/sensory nerves are injected. Sensory complications are significantly less or nonexistent when pure motor nerves such as the obturator nerve (hip adductors) or musculocutaneous nerve (biceps) are treated. Intramuscular hematomas can form.
The local effects of the hematoma can negate the benefits of the injection. In addition, large doses of phenol delivered into the systemic circulation can lead to tremors, convulsions, and cardiorespiratory collapse.
If administered incorrectly or in subcutaneous muscles there may be erythema, blistering and potential skin slough.
Morrison JE Jr, Hertzberg DL, Gourley SM, et al. Motor point blocks in children. A technique to relieve spasticity using phenol injections. AORN 1989;49:1346-51.
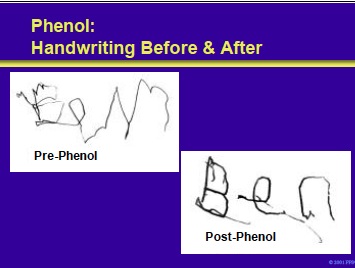
This is an example of the improvement in fine motor skills that resulted from phenol neurolysis in a child with cerebral palsy
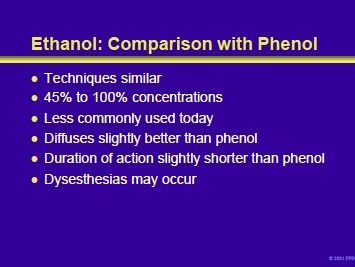
Ethanol neurolysis has also been employed to treat focal spasticity, although less commonly. Injections of 45% to 100% ethanol are performed with electrode stimulation in the same fashion as with phenol.
Ethanol diffuses slightly better than phenol with a slightly shorter duration of action. As with other neurolytic agents, dysesthesias may occur following injection of mixed motor/sensory nerves.
- Next section : Management of spasticity in cerebral palsy Part VIII -Botulinum Toxin
Add comment