- Lectures / Webinars
- 11. Alternative Medicine in Spasticity Management
11. Alternative Medicine in Spasticity Management
Hot 
Alternative medicine appears to be an increasingly popular option among physicians and patients. With the availability of a large amount of anecdotal material and non-peer reviewed information over the Internet, the physician managing patients with cerebral palsy and spasticity should be aware of some of the alternative medical approaches to spasticity and their evidence base.

Alternative medicine is a non-orthodox therapeutic system that has no satisfactory scientific explanation for the treatment’s effectiveness. The term covers a large spectrum of healing philosophies, approaches, and therapies (eg, acupuncture, herbs, homeopathy). Alternative medicine is not taught in medical schools and is without a strong evidence base for efficacy.
When evaluating alternative medical approaches for cerebral palsy and other disorders, the physician should consider the following points:
- What is the physiological/pharmacological basis for the intervention?
- Is there an evidence base for employing an alternative approach?
- Is the approach associated with significant risks to the patient?
- What are the cost implications of a specific alternative medical therapy?
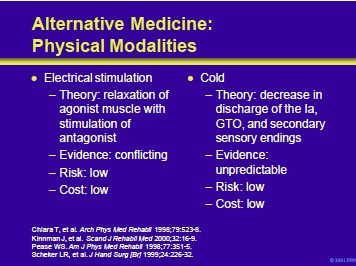
Electrical stimulation has been employed in the management of spasticity in patients with cerebral palsy and other disorders of the central nervous system. Physiologically, improvement in motor function might follow stimulation that triggered spastic muscles and inhibited antagonists.
The evidence for this approach is conflicting. In one study of a patient with spastic paraparesis who failed trials of physical therapy and baclofen, quantitative gait analysis demonstrated improvement following electrical stimulation of the quadriceps and anterior compartment musculature.
In a trial of 19 patients with spastic cerebral palsy, electrical stimulation of the antagonist extensors for 3 to 43 months, combined with dynamic bracing, dramatically decreased the manifestations of spasticity. The risks and costs of this intervention are low.
Topical cold may decrease reflex activity for short periods pres umably secondary to a decrease in neuronal discharges from different sources. However, the evidence for this approach is conflicting.
One study found statistically significant, but clinically irrelevant, changes in spasticity with a cooling suit. Another study found a weak, but significant, correlation between temperature decrements and reduction of central motor conduction. The risks and costs of this intervention are low.
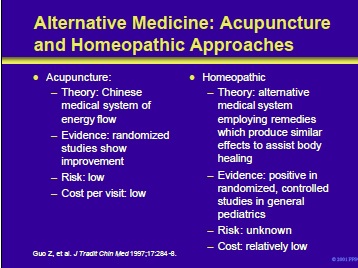
Acupuncture is the ancient Chinese medical system of energy flow. Production of needling sensations is believed to alter the energy flow and restore homeostasis. Randomized studies of this approach in patients with spasticity are said to show improvement.
The risks and cost-per-visit are low. Homeopathic medicine attempts to heal by employing remedies which produce similar effects to assist the healing process (eg, the administration of ipecac in minute doses to heal a woman with morning sickness).
Evidence for this approach is said to be positive in randomized, controlled studies in the pediatric population with cerebral palsy. The risks are unknown and costper- visit are low.
Guo Z, Zhou M, Chen X, et al. Acupuncture methods for hemiplegic spasm. J Tradit Chin Med 1997;17:284-8.

Kava Kava is a South Pacific herb that was largely unknown in the United States until 1996 when a group of 21 herbal product makers designed a plan to aggressively market it. Kava has been marketed as an anxiolytic. The active ingredient is a kavalactone that may upregulate GABA receptors. Research on the efficacy of kava in patients with cerebral palsy and spasticity is anecdotal.
Psychological addiction can occur and there is a potential for drug-interactions. However, the cost of this intervention is low. Hyperbaric oxygen can be used to increase oxygenation of hypoxic, watershed areas that may be contributing to the process.
Research is limited and predominantly anecdotal. However, in a study of 25 children with diplegic cerebral palsy, treatment produced an improvement in both gross and fine motor movement as well as decreasing spasticity.
Risks include middle-ear problems and a potential to interfere with the delivery of intrathecal baclofen. Costs of this intervention are high and require a center with the proper equipment.

Based on study results of animals with upper motoneuron lesions, Taub et al focused on the use of constraint-induced training. Notably, patients eligible for this approach have some use of the extremity before intervention. The efficacy of this approach has been demonstrated by Crocker et al in a child with spastic cerebral palsy.
The non-involved hand was placed in a splint to force the child to use the affected extremity. The patient demonstrated increased use of the spastic extremity in free play, eating, and with standardized tests of fine motor skill.
Crocker MD, MacKay-Lyons M, McDonnell E. Forced use of the upper extremity in cerebral palsy: a single-case design. Am J Occup Ther 1997;51: 824-33.
Taub E, Miller NE, Novack TA, et al. Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil 1993;74:347-53.
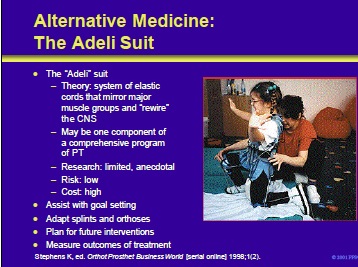
The “Adeli” suit is an adaptation of the Russian cosmonauts’ space uniforms. It was originally developed to combat hypokinesis during episodes of extended weightlessness. The suit consists of a system of adjustable elastic cords attached to a wide belt worn at the hip and joint area and connected with shoes and knee pads.
The system of elastic connectors topographically mirrors the arrangement of flexor and extensor muscles, trunk rotators and lower limbs. It works as an elastic frame around the body and is said to help “rewire” and retrain the central nervous system as feedback from properly aligned and moving muscles is received by the brain.
For example, if a child walks on tiptoes, the bands in the toes are tightened forcing the child to take full-footed steps. At this time, the evidence base for the “Adeli” suit is limited and anecdotal. The risks of the intervention are low and the costs for acquisition and fitting the suit are high.
Stephens K, ed. Poland: Space suit technology offers new hope for cerebral palsy rehab. Orthot Prosthet Business World [serial online]. Spring 1998;1(2). Accessed December 15, 2000.

Alternative medicine options in children with cerebral palsy and spasticity include:
- Conductive education
- Craniosacral manipulation
- Patterning
- Other options
Alternative medicine appears to be an increasingly popular option among physicians and patients. With the availability of a large amount of anecdotal material and non-peer reviewed information over the Internet, the physician managing patients with cerebral palsy and spasticity should be aware of some of the alternative medical approaches to spasticity and their evidence base.
Cerebral palsy is a group of disorders of motion and posture. It may be due to prenatal, perinatal, or postnatal disorders. Prior to initiation of therapy, the child with CP should be carefully evaluated by a team of specialists including neurologists, orthopedic surgeons, physiatrists, pediatricians, occupational therapists, physical therapists and speech pathologists.
The examination should include tests of active and passive range of motion. In addition, one or more standardized tests of function and disability should be included to gauge the success of the therapeutic interventions. Therapeutic options in the child with cerebral palsy and spasticity include pharmacotherapy, rehabilitation therapy and surgical interventions (orthopedic and neurosurgical).
Pharmacological agents can be used to modulate the manifestations of generalized spasticity.
Neurolytics (eg, phenol) and chemodenervation with BTX offer the opportunity to specifically target spastic muscles and improve functional status.
Surgical interventions can correct anatomic abnormalities resulting from spasticity and interrupt neuroanatomical pathways that contribute to the clinical manifestations.
Rehabilitation management in the child with cerebral palsy is a tool to increase motor control, improve function in activities of daily living and improve quality of life. The role of some alternative medical approaches in the treatment of spasticity is intriguing but lacks a clear evidence base in most instances.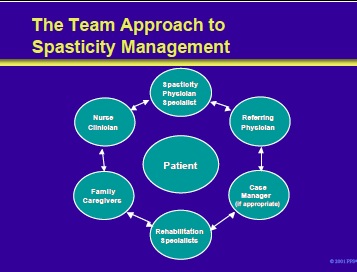
The team approach to the management of spasticity in children with cerebral palsy is centered about the patient.
Core team members include:
- Spasticity physician specialists
- Referring physician
- Rehabilitation specialists
- Family/caregivers
- Nurse clinicians
- Case manager (if appropriate)
- See Next section Management of spasticity in cerebral palsy Part XII Case Studies
Add comment