- Lectures / Webinars
- 2. Management of spasticity in cerebral palsy Part II Passive and Active Examination
2. Management of spasticity in cerebral palsy Part II Passive and Active Examination
HotThis section will discuss the passive and active examination of the child with cerebral palsy
Inspection of gait
The patient must be studied carefully while walking. The clinician should look at the entire gait including all joints. Since some of the tendons attached to the muscles are subcutaneous, a good clinical examination can often determine their activity. The gait can also be recorded on videotape.
Lower Extremity: Hip Range of Motion
{jwplayer}&file=mos/LowerExtHipRange_MP4+512Kbps.mp4&streamer=rtmp://s17ewxq9sfv3xv.cloudfront.net/cfx/st&provider=rtmp{/jwplayer}
Hip flexion is measured with the child supine. The Thomas test is performed by flexing both hips to eliminate the lumbar lordosis. One of the hips is extended and the other is flexed. This is a measure of hip flexion contracture.
Lower Extremity: Staheli Test
{jwplayer}&file=mos/STAHEL1_MP4+512Kbps.mp4&streamer=rtmp://s17ewxq9sfv3xv.cloudfront.net/cfx/st&provider=rtmp{/jwplayer}
The child is placed in a prone position with the pelvis at the edge of the examination table. One of the hips is extended until the pelvis moves. This is another measure of the hip flexion contracture
Lower Extremity: Hip Abduction
{jwplayer}&file=mos/Hipabduc_MP4+512Kbps.mp4&streamer=rtmp://s17ewxq9sfv3xv.cloudfront.net/cfx/st&provider=rtmp{/jwplayer}
Hip abduction is measured with the hips flexed (to remove the influences of the hamstring muscles) and with the hips extended.
Lower Extremity: Internal and External Rotation of Hip
{jwplayer}&file=mos/INTERN1_MP4+512Kbps.mp4&streamer=rtmp://s17ewxq9sfv3xv.cloudfront.net/cfx/st&provider=rtmp{/jwplayer}
In a prone position the hips are internally and externally rotated
Lower Extremity: Popliteal Angle
{jwplayer}&file=mos/POPLIT1_MP4+512Kbps.mp4&streamer=rtmp://s17ewxq9sfv3xv.cloudfront.net/cfx/st&provider=rtmp{/jwplayer}
With the patient in a supine position, the hip is flexed to 90 degrees. The knee is then extended as far as possible. The angle from full extension to the tibia is measured (a positive or negative number) or the angle made by the femur and tibia is measured. This is a measure of hamstring contracture.
Lower Extremity: Quadriceps Tests
{jwplayer}&file=mos/PRONEK1_MP4+512Kbps.mp4&streamer=rtmp://s17ewxq9sfv3xv.cloudfront.net/cfx/st&provider=rtmp{/jwplayer}
In a prone position the knee is rapidly flexed. The Ely-Duncan test is a measure of spasticity of the rectus femoris muscle. A slow flexion is a measure of a contraction of the rectus femoris muscle
Lower Extremity: Ankle Range of Motion
{jwplayer}&file=mos/SILFVE1_MP4+512Kbps.mp4&streamer=rtmp://s17ewxq9sfv3xv.cloudfront.net/cfx/st&provider=rtmp{/jwplayer}
The ankle dorsiflexion is measured with the knee in flexion and extension. In extension, contracture of both the gastrocnemius and soleus muscles are measured, while in knee flexion only the soleus is measured. The foot should be supinated to measure only ankle motion as supination locks the subtalar and midfoot joints.
Physical examination should include observation of upper extremity function with the patient sitting and, if appropriate, during activity or walking. Patterns of movement should be noted and the presence of movement disorders should be characterized (eg, athetosis, dystonia). Movement disorders are a relative contraindication to operative interventions on the upper extremity and can result in opposite deformities (eg, the “athetoid shift”). The examination should also include an assessment of sensibility, measurements of active and passive range of motion and an assessment of the degree of spasticity by the Ashworth Scale, the Modified Ashworth Scale or the Tardieu Scale.
Common upper extremity defects in patients with cerebral palsy include:
- Internal rotation of the shoulder
- Elbow flexion
- Forearm pronation
- Wrist flexion
- Finger flexion
- Thumb-in-palm deformity
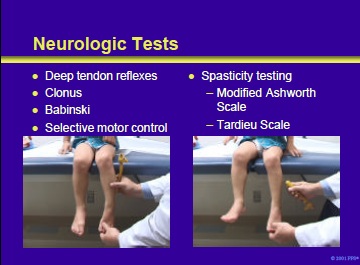
Testing deep tendon reflexes permits an adequate sampling of reflex activity of the spinal cord and ensures that the reflex arcs are intact. Hyperreflexia is a characteristic of spasticity.
Clonus can be elicited by sudden stretch of the target muscle. It manifests as rhythmic, uniphasic or monophasic contractions and relaxations of a group of muscles.
Babinski: The plantar reflex is elicited when the sole of the foot is stimulated on its lateral border from heel to toe. A positive Babinski sign consists of dorsiflexion of the great toe with splaying of the digits. It is a manifestation of an upper motoneuron lesion. Selective motor control should also be evaluated for both gross and fine muscles of the extremities.
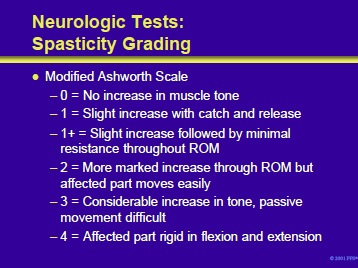
Several measures can be used to grade spasticity and follow the results of treatment. These include:
- Ashworth Scale
- Modified Ashworth Scale
- Tardieu Scale
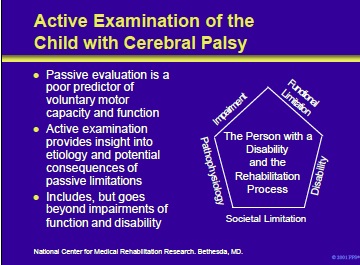
Passive evaluation is a poor predictor of a patients voluntary motor capacity and function. Active examination, on the other hand, explores the etiology and potential consequences of passive limitations. As such, it extends the evaluation to function and disability.
The National Center for Medical Rehabilitation Research (NCMRR) graphic in the right panel of this slide illustrates the inclusive approach taken by the active examination process.
Dimensions of disablement include:
- Pathophysiology: Interruption or interference of normal physiology and developmental processes or structures
- Impairment: Loss or abnormality of body structure or body function
- Functional Limitation/Activity: Restriction of ability to perform activities
- Disability/Participation: Restricted participation in typical societal roles
- Societal Limitation/Context: Barriers to full participation imposed by societal attitudes, architectural barriers and social policies and other external factors
National Center for Medical Rehabilitation Research, Executive Building, Room 2A03, 6100 Executive Boulevard, MSC 7510, Bethesda, MD, 20892-7510; (301) 402-2242.
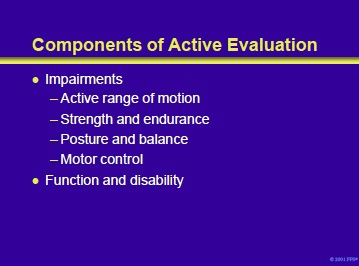
Components of active evaluation include impairment, function and disability.
Methods to measure impairments include the following:
- Range of motion can be assessed by adding an active component to the passive motion exam and measure range with a goniometer or with a 3-D kinematic gait analysis to quantify motion during gait and other tasks.
- Strength and endurance can be evaluated through posture and motion, fatigability, functional tests, isometric or isokinetic dynamometry, oxygen or heart rate, or instrumented activity monitoring (eg, step activity monitor).
- Posture and balance can be assessed by direct observation of static and dynamic posture, specific tests or protocols, kinematic record of static posture, indicators from gait such as limb support times and step width, or force plate (sway) and instrumented balance systems.
- Motor control can be evaluated by observing isolated movements without gravity and with adjacent joints in flexion and extension; observing intralimb and interlimb patterns; kinematic analyses of active motion under different conditions and EMG analyses of muscle activation during tasks.
Standardized tools are used to assess function and disability in patients with cerebral palsy. The measuring tools are highly specific with detailed instructions to guide assessment, scoring and interpretation.
They are typically developed with a large sample of children whose performance will be the standard of comparison. They are then developed and modified through a rigorous process to ensure psychometric integrity.
Failure to use the standard measures to assess function and disability may result in the following:
- Variations in observations across assessments (ie, memory is not very reliable)
- Errors of omission and commission in gathering evidence
- Tendency to record “impressions” rather than evidence
- Tendency to focus on impairment deficits rather than functional performance
Considerations when selecting an instrument include:
- Goals of the assessment
- Aspects to be measured
- Intended population
- Age-span covered by the instrument
- Intended range in level of involvement
- Any need for special equipment and training
- Ease of scoring and interpretation
- Clinical usefulness of results
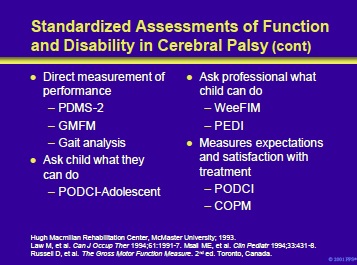
Direct measurements of performance include:
- Peabody Developmental Motor Scales (PDMS-2): This is a revised “throw-back” to long-standing developmental motor tests. Its normative sample and validation are impressive; however, it is only for young children.
- Gross Motor Function Measure (GMFM): This is a clinicianadministered test of gross motor function that quantifies how much motor function a child can demonstrate in a structured setting. It is objective and reliable and takes <1 hour to administer and score; however, it shows a ceiling effect for more functional children.
- Gait analysis: see following section
Measurement of what the child says they can do:
- Pediatric Outcomes Data Collection Instrument (PODCIAdolescent): This measure is framed from the family perspective, not that of the physician. Evaluates global function, expectations, happiness, satisfaction with symptoms. This instrument fills a large void in pediatric rehabilitation and evaluates a child with a disability in the context of everyday life; however, manual scoring is cumbersome and questions may not be appropriate for nonambulatory children.
Ask the professional what the child can do:
- Pediatric version of the Functional Independence Measure (WeeFIM): This instrument is a general inventory of health status that can be completed by one or more professionals. It is a simple, well-established test; however, it shows a ceiling effect for less involved children.
- Pediatric Evaluation of Disability Inventory (PEDI): The PEDI is a new functional assessment instrument for the evaluation of disabled children aged 6 months to 7 years. The PEDI has been developed to identify functional status and change along three dimensions: (1) functional skill level, (2) caregiver assistance and (3) modifications or adaptive equipment used.
Measures the expectations and satisfaction with treatment:
- Pediatric Outcomes Data Collection Instrument (PODCI): See above
- Canadian Occupational Performance Measure (COPM)
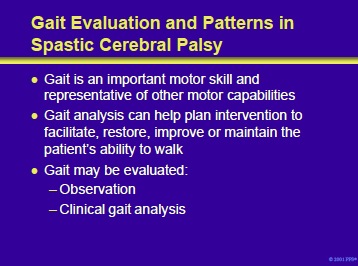
Gait is a series of multiple limb segment rotational movements that produce stable forward propulsion in an energy-conserving manner. It is an important motor skill and representative of other motor capabilities.
Although a number of atypical gait patterns have been described in patients with cerebral palsy, each patient has a unique set of impairments, functional limitations and associated compensations producing these patterns. Therefore, the mechanisms operative for an individual patient should be determined and are the basis for directing a tailored rehabilitation program.
Gait is studied in patients with cerebral palsy so that interventions can facilitate, restore, improve or maintain the patient’s ability to walk. Gait may be evaluated either observationally or with clinical gait analysis. Physicians commonly describe gait based upon observations during the initial and subsequent examinations.
However, it is often difficult to appreciate all limb segment and joint motions through different phases of the gait since all limbs and joints are moving at the same time in three-dimensional space. Therefore, observational gait evaluation can be supplemented by videotape taken while the patient is walking. Quantitative gait analysis is a particularly useful tool for developing a treatment plan.
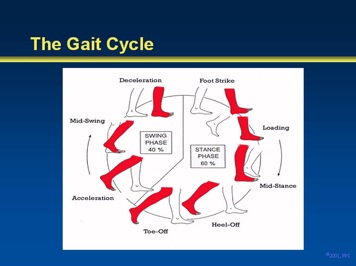
The gait cycle begins with floor contact by one foot and ends with the next consecutive floor contact of that same foot. This graphic illustrates the various phases of the gait cycle.
Components include:
- Foot strike
- Loading response
- Mid-stance
- Heel-off
- Toe-off
- Acceleration
- Midswing
- Deceleration
The foot strike through toe-off is considered the stance phase and comprises 60% of the cycle. The remaining elements constitute the swing phase.
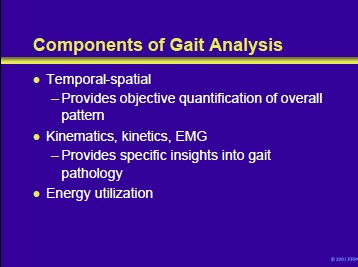
Gait analysis can be divided into temporal-spatial and kinematic, kinetic, and EMG analyses. Modern-day gait analysis quantitatively analyzes gait with a sophisticated computerized video apparatus that measures and digitally records the three-dimensional location of individual markers throughout the gait cycle. The temporal-spatial relationship recorded provides objective quantification of the overall pattern.
Kinematics assesses joint range of motion during gait. Notably, however, they provide only relative joint angle information, not absolute positions of each joint segment. Kinetics calculates the joint power (force) associated with gait.
Dynamic electromyography measures the timing and magnitude of muscle activity during walking with either surface electrodes or fine wires inserted into muscles. These tools provide additional specific insights into gait pathology.
Energy utilization can be measured by oxygen utilization, oxygen cost and heart rate monitoring.
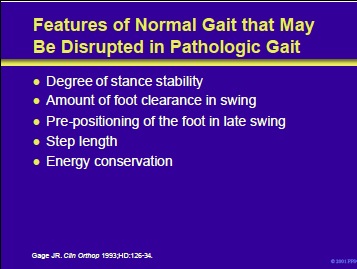
Potential areas in which abnormalities could lead to a pathologic gait are listed on the slide and include:
- Stability of stance
- The amount of foot clearance in swing
- Appropriate pre-positioning of the foot in late swing
- Adequate step length
- Energy conservation
Gage JR. Gait analysis: an essential tool in the treatment of cerebral palsy. Clin Orthop 1993;HD:126-34.
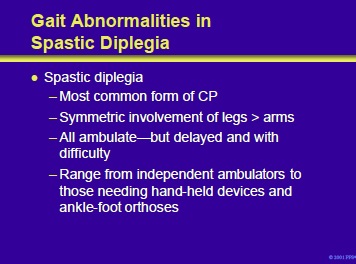
Spastic diplegia is the most common form of cerebral palsy. It presents with symmetric involvement of the legs and arms. All patients eventually ambulate, but walking is delayed and difficult. The degree of difficulties with gait in patients with spastic diplegia range from independent ambulators to those patients requiring hand-held devices and ankle-foot orthoses.
Temporal-spatial and EMG features of spastic diplegia are beyond the scope of this slide kit.
However, useful kinematic features of the gait in a patient with the classic form of spastic diplegia include:
- Forefoot strike with early heel rise
- Increased knee flexion
- Adduction and internal rotation of the hip
- Stiff-knee gait
- Excessive lumbar lordosis
- Increased hip flexion
This slide illustrates some of the characteristic abnormalities of gait, mentioned in the notes on the previous page, in a patient with spastic diplegia.
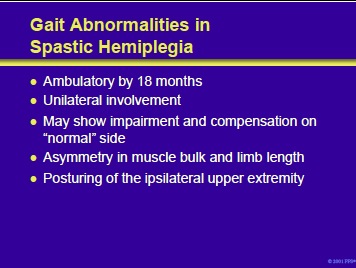
Patients with spastic hemiplegia are usually ambulatory by the age of 18 months and show a unilateral abnormality of gait. It is important to carefully observe the “normal” side since the patient may also manifest either subtle or compensatory alterations on this side. As a consequence of the hemiplegia, these patients will have asymmetry in muscle bulk and limb length.
Temporal-spatial and EMG features of spastic hemiplegia are beyond the scope of this slide kit.
However, useful kinematic features of the gait in patients with spastic hemiplegia include:
- Toe strike
- Flexion of the hip and knee or knee recurvatum
- Pelvic retraction and elevation
- Greater knee flexion or vaulting on the contralateral side
- Posturing of the ipsilateral upper extremity
Gait Abnormalities in Spastic Hemiplegia
{jwplayer}&file=mos/CHILDP1_MP4+512Kbps.mp4&streamer=rtmp://s17ewxq9sfv3xv.cloudfront.net/cfx/st&provider=rtmp{/jwplayer}
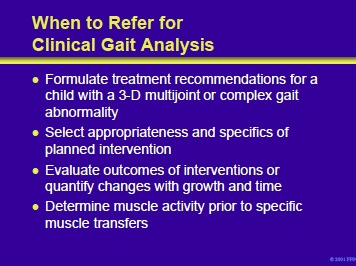
Patients with cerebral palsy should be referred for gait analysis when they have three-dimensional multijoint or complex abnormalities of gait that complicate the treatment plan. Gait analysis should be performed before aggressive interventions to aide in the evaluation and appropriateness of the selected procedure(s). Clinical gait analysis can also be used to evaluate outcomes of interventions or quantify changes over time and to determine muscle activity prior to orthopedic interventions that transfer muscles.

A number of gait-specific considerations are important when considering treatment. The specific muscles and joints that are involved in the gait disturbance should be identified; in addition, it is important to determine the plane of movement affected. Since some of the gait abnormalities may be the result of compensatory mechanisms rather than spasticity per se, it is important to recognize the differences.
Furthermore, the therapist should avoid exacerbating the situation by creating weakness or opposite deformity. The therapeutic goal is not a “normal” gait. Instead, the objective is a more stable gait that is produced with less effort and oxygen consumption and that minimizes joint damage over the longterm.
Next Section : Management of spasticity in cerebral palsy Part III Treatment of Patients with cerebral palsy and spasticity
Section Index
- Management of spasticity in children with cerebral palsy Part I
- Management of spasticity in cerebral palsy Part II Passive and Active Examination
- Management of spasticity in cerebral palsy Part III Treatment of Patients with cerebral palsy and spasticity
- Management of spasticity in cerebral palsy Part IV - Rehabilitation Management
- Oral Medications for the Treatment of Spasticity
- Intrathecal Baclofen for Spasticity in Cerebral Palsyy
- Local Anesthetics, Neurolytics, and Chemodenervation for the Patient with Cerebral Palsy and Spasticity
- Management of spasticity in cerebral palsy Part VIII -Botulinum Toxin
- Neurosurgical Interventions for Spasticity in Children with Cerebral Palsy
- Orthopedic Interventions for Spasticity in Children with Cerebral Palsyy
- Management of spasticity in cerebral palsy Part XI-Alternative Medicine in Spasticity Management
- Management of spasticity in cerebral palsy Part XII Case Studies
- Management of spasticity in cerebral palsy Part XIII Document Downloads
- Self Assessment
Add comment