- Lectures / Webinars
- 10. Orthopedic Interventions for Spasticity in Children with Cerebral Palsy
10. Orthopedic Interventions for Spasticity in Children with Cerebral Palsy
HotCerebral Palsy

Both orthopedic and neurosurgical interventions can be used to treat the consequences of upper motoneuron lesions in patients with cerebral palsy.
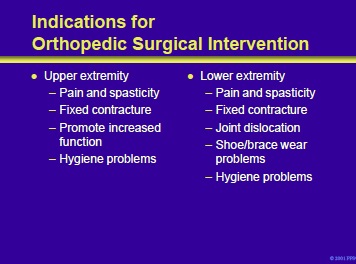
Indications for orthopedic intervention in patients with cerebral palsy and upper extremity spasticity include:
- Pain and spasticity
- Fixed contracture
- Promote increased function
- Hygiene problems
Indications for orthopedic intervention in patients with cerebral palsy and lower extremity spasticity include:
- Pain and spasticity
- Fixed contractures
- Joint dislocation
- Shoe/brace wear problems
- Difficulties maintaining hygiene
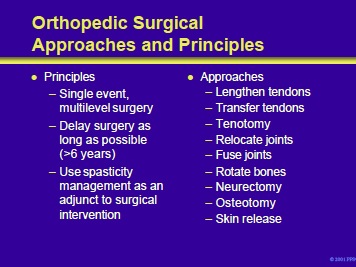
Principles of orthopedic surgery on patients with cerebral palsy and spasticity include the following:
- Single event, multilevel surgery
- Delay the operation for as long as possible, preferably until a child is at least 6 years old.
- Use spasticity management tools as an adjuvant to surgical intervention.
A variety of surgical techniques can be used to help correct the static and dynamic defects that occur in the patient with cerebral palsy and spasticity. These include:
- Procedures to lengthen, transfer, or divide tendons
- Relocate joints
- Fuse joints
- Rotate bones
- Transect specific nerves, correct bony abnormalities, and release contracted skin.
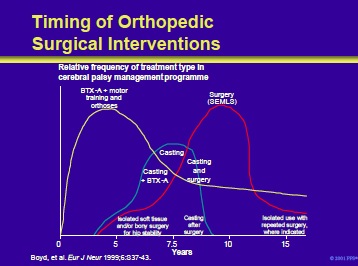
This slide illustrates an integrated plan for the management of patients with cerebral palsy and spasticity that encompasses chemodenervation with BTX, orthoses, casting, and orthopedic surgery.
Boyd, et al. Eur J Neur 1999;6:S37-43.
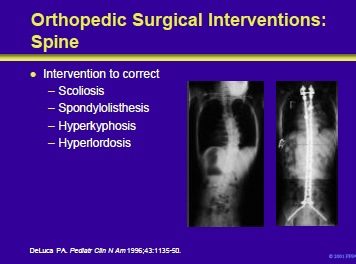
Scoliosis, spondylolisthesis, hyperkyphosis and/or hyperlordosis in patients with cerebral palsy create difficulties in maintaining a seated position and, in patients with severe forms, can produce obliquity of the pelvis, ischial pressure sores and cardiopulmonary compromise. Management of scoliosis by bracing is less successful in halting progression in patients with cerebral palsy than in idiopathic forms.
However, bracing can be used to delay the need for surgery in the very young. When curves progress to >40 degrees and lose their flexibility, some form of segmental instrumentation is indicated (as shown in this slide).
DeLuca PA. The musculoskeletal management of children with cerebral palsy. Pediatr Clin N Am 1996;43:1135-50.
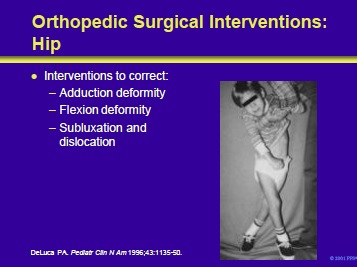
Orthopedic surgical interventions can be used to correct defects of the hip in patients with cerebral palsy. Potential problems include adduction deformity, flexion deformity, subluxation and dislocation.
In patients with an established dislocation of the hip, it is better to have a dislocated, mobile hip than one that is located but painful. Therefore, intervention should be considered only when the dislocation is recent and not accompanied by severe deformity of the femoral head or acetabular dysplasia.
The patient illustrated in the right panel has a hip adduction deformity. Interventions that might be employed in this patient include open or percutaneous lengthening of the adductors and/or an obturator neurectomy.
DeLuca PA. Common orthopedic problems II: the musculoskeletal management of children with cerebral palsy. Pediatr Clin N Am 1996;43:1135-50.
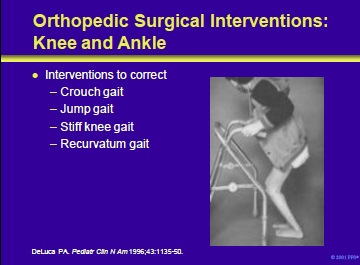
Orthopedic surgical intervention can be used to correct abnormalities of the ankle and knee in patients with cerebral palsy.
Potential problems include:
- Crouch gait is usually iatrogenic.It is recognized by increased hip flexion, increased knee flexion and increased ankle dorsiflexion.
- Jump gait is seen in patients with diplegia or hemiplegia. It is recognized by increased hip flexion, increased knee flexion and increased ankle plantar flexion.
- Stiff knee gait is manifested by swing phase knee stiffness and results in problems with foot clearance. Patients attempt to compensate by hip circumduction, external rotation and contralateral vaulting.
- Recurvatum gait is usually iatrogenic. It is difficult to treat surgically and often requires long leg braces.
The patient shown in the right panel of this slide has a crouch gait. This presentation is common in patients with cerebral palsy and results from hamstring spasticity. It may be exacerbated by prolonged positioning in a seated position. It can be improved by hamstring lengthening.
This video illustrates characteristics of the “crouch” gait.
This video illustrates characteristics of the “jump” gait.
This video illustrates characteristics of the “stiff knee” gait.
This video illustrates characteristics of the “recurvatum” gait.
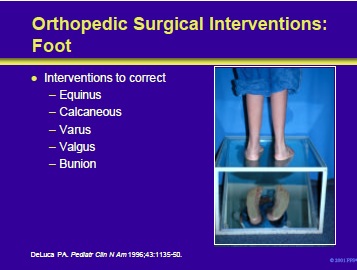
Orthopedic surgical interventions can be used to correct abnormalities of the foot in patients with cerebral palsy.
Potential problems include:
- Equinus
- Calcaneous
- Varus
- Valgus
- Bunion
The patient shown in the panel on the right has a varus foot. It is usually seen in patients with hemiplegia.
Surgical options include:
- Frost lengthening of the posterior tibialis muscle
- Split posterior tibialis tendon transfer (SPOTT)
- Split anterior tibialis tendon transfer (SPLATT)
DeLuca PA. Common orthopedic problems II: the musculoskeletal management of children with cerebral palsy. Pediatr Clin N Am 1996;43:1135-50.
Upper extremity involvement is present in approximately 80% of patients with cerebral palsy. Orthopedic surgical intervention can be used to correct abnormalities of the upper extremity in these patients.
Potential problems include:
- Shoulder internal rotation
- Wrist and elbow flexion contractures
- Thumb adduction contractures
- “Swan-neck” deformities of the fingers
- Forearm pronation
- Thumb-in-palm
The surgical concepts related to this complex neurologic problem must be kept rather simple, and include principally the release of spastic deforming muscles, and, secondly, the use of augmentation tendon transfers to maintain an improved functional position.
The most important aspect of surgical planning is to assess whether or not the individual is attempting to use the upper extremity voluntarily. In patients that are, surgical procedures can reposition the deformed limb and enable the patient to function more effectively.
Alternately, it is most important to understand that an orthopedic intervention will not stimulate an individual to begin to use a previously functionless limb.
DeLuca PA. Common orthopedic problems II: the musculoskeletal management of children with cerebral palsy. Pediatr Clin N Am 1996;43:1135-50.
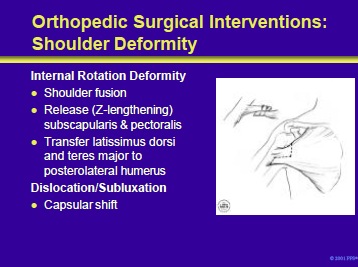
Shoulder internal rotation deformity may be managed by shoulder fusion in severe cases. In less severe cases in which there is dynamic instability, release or lengthening of the subscapularis and/or pectoralis major will improve passive range of motion. Transfer of the latissimus dorsi and teres major to the posterolateral humerus will improve active external rotation. (The panel on the right shows Z-lengthening of the pectoralis major.)
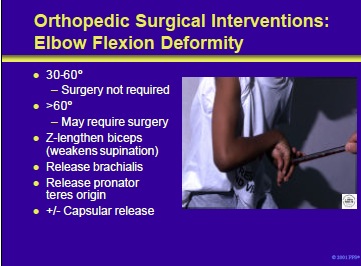
Surgery of the elbow is not usually required in patients with contractures of 30 to 60 degrees. Contractures greater than 60 degrees, which interfere with function or hygiene, may be improved with surgical intervention.
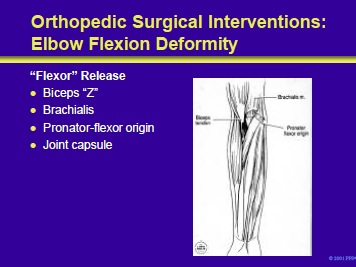
Flexion deformity may be improved by Z-lengthening of the biceps, release of the brachialis, release of the pronator-flexor origin and/or release of the elbow joint capsule.
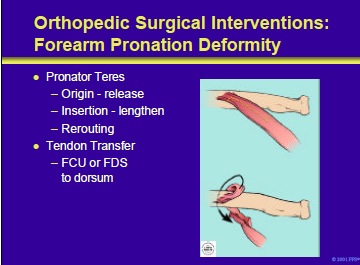
Pronation deformity in patients with cerebral palsy may be managed by release of the origin, lengthening of the insertion or rerouting of the pronator teres to provide active supination. Tendon transfers to the dorsum to the wrist to improve wrist extension can augment supination by appropriate routing. The picture on the right demonstrates a technique of re-routing the distal pronator around the radius to create supination.
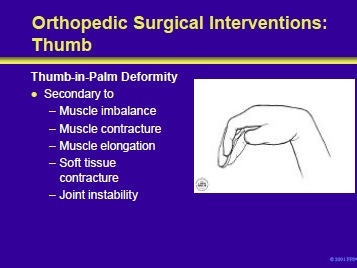
Thumb-in-palm deformity is multifactorial and includes intrinsic and extrinsic muscle imbalance, contracture of skin and myotendinous structures, elongation of extensor muscles and tendons, contracture of flexor muscles and tendons, soft tissue contracture, joint instability and weakness.
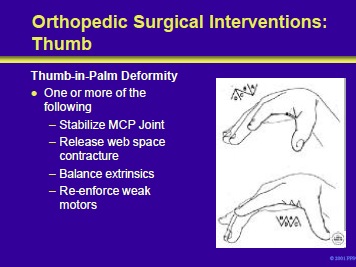
Thumb-in-palm deformity may require multiple procedures including MCP stabilization with fusion or capsulodesis, release of web contracture, release or lengthening of contracted tendons, plication of elongated structures and tendon transfer to improve strength.
- See Next Section : Management of spasticity in cerebral palsy Part XI-Alternative Medicine in Spasticity Management
Add comment