- Lectures / Webinars
- 7. Neurosurgical Interventions for Spasticity in Children with Cerebral Palsy
7. Neurosurgical Interventions for Spasticity in Children with Cerebral Palsy
Hot
Both orthopedic and neurosurgical interventions can be used to treat the consequences of upper motoneuron lesions in patients with cerebral palsy.
Neurosurgical interventions in a patient with cerebral palsy and spasticity include:
- Selective dorsal rhizotomy (SDR): section of sensory nerve roots disrupts the reflex arcs and decreases tone. This procedure does not affect dyskinesias.
- Peripheral neurectomy: this procedure can be used to manage spasticity in selective muscle groups (eg, obturator neurectomy in patients with hip adduction deformity).
- Myelotomy: a neurosurgical procedure that interrupts reflex arcs by surgically dividing the cord from T12 to S1 into ventral and dorsal portions.
- Dorsal column electrical stimulation: stimulation of the dorsal columns by an epidural electrode can be used to decrease tone.
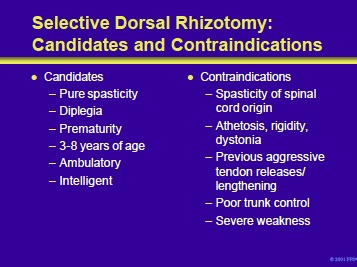
The ideal candidates are purely spastic with the majority of their involvement in the legs. Children born prematurely tend to fit into the ideal category most commonly. The above are not absolute criteria since many children that do not meet the criteria on the slide may still respond positively to the procedure. Rhizotomy typically does not affect spinal cord origin spasticity or dyskinesias (eg, athetosis, rigidity).
If the patient has had previous aggressive tendon releases or lengthening, excess weakness can occur and may not be recoverable. Trunk control can decrease temporarily and patients who undergo the procedure with impaired trunk control may worsen after the intervention.
Patients with poor selective motor control may also not benefit.
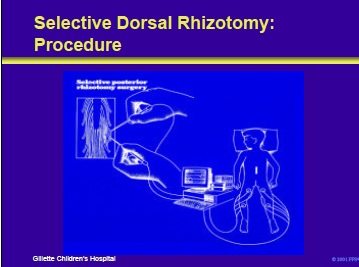
This slide illustrates the procedure. The dorsal roots of L2 to S2 are exposed. Rootlets are teased out with a nerve hook and then stimulated individually. If there is an abnormal EMG or muscle activity, the nerve rootlet is cut. In most instances, 25% to 40% of all rootlets are cut. The procedure may produce temporary, and occasionally complete, anesthesia or dysesthesias.
In aggressive procedures, in which 60% of the rootlets are sectioned, severe sensory loss can occur. In most instances, the patient is very weak for the first several weeks or months following the procedure with a resultant decreased function. However, strength does recover to a presurgery level. Infection, weakness, and scoliosis can all complicate the procedure.
Chambers HG. The surgical treatment of spasticity. Muscle Nerve 1997;20(suppl 6):S121-8.
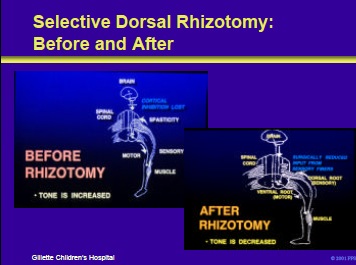
Loss of cortical inhibition allows afferent impulses from muscle spindles to produce hypertonicity and spasticity. Following rhizotomy, tone is decreased because the afferent input from muscle spindles cannot reach the cord to stimulate the alpha motoneurons.
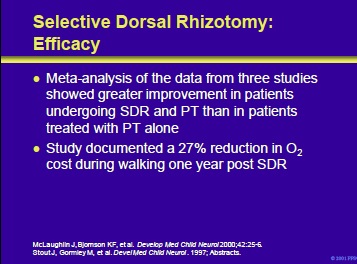
A number of studies have analyzed the therapeutic efficacy of SDR and physical therapy (PT) compared to PT alone. A recent meta-analysis of the data from three studies provided evidence that patients undergoing SDR plus PT did better than PT alone. Stout et al evaluated oxygen cost (energy efficiency) with walking in patients who underwent a SDR.
One year after the procedure, operated patients showed a 27% reduction in O2 cost. Patient selection is the key to optimum outcome. In properly chosen patients, results of SDR can be better than other antispasticity approaches.
McLaughlin J, Bjornson KF, Temkin N, et al. Selective dorsal rhizotomy: meta-analysis of three randomized clinical trials. Develop Med Child Neurol 2000;42:25-6.
Stout J, Gormley M, et al. The effects of selective dorsal rhizotomy on oxygen consumption and gait velocity in children with cerebral palsy. Devel Med Child Neurol. 1997; Abstracts.
- See Next section: Orthopedic Interventions for Spasticity in Children with Cerebral Palsy
Add comment