 A study led by Brian McCabe and his team from the Motor Neuron Center at Columbia University Medical Center (CUMC) suggests that contrary to existing theories, Spinal muscular atrophy (SMA), results primarily from motor circuit dysfunction and not motor neuron or muscle cell dysfunction
A study led by Brian McCabe and his team from the Motor Neuron Center at Columbia University Medical Center (CUMC) suggests that contrary to existing theories, Spinal muscular atrophy (SMA), results primarily from motor circuit dysfunction and not motor neuron or muscle cell dysfunction
SMA, a hereditary neuromuscular disease characterized by muscle atrophy and weakness is caused by defects in a gene called SMN1 (survival motor neuron 1), which encodes the SMN protein.
There are several forms of SMA, distinguished by time of onset and clinical severity. The most severe form, Type 1, appears before six months of age and generally results in death by age two. In milder forms, symptoms may not appear until much later in childhood or even in early adulthood. There is no treatment for SMA, which is estimated to affect as many as 10,000 to 25,000 children and adults in the United States and is the leading genetic cause of death in infants.
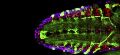
The researchers studied1 Drosophila (Fruit Flies) SMN mutants which had been genetically altered so that every cell had a defective copy of the SMN1 gene. The mutant flies had reduced muscle size and defective locomotion, motor rhythm, and motor neuron neurotransmission. When fully functional copies of SMN1 were introduced into the flies' motor neurons or muscle cells, the cell types previously thought to be affected, the flies unexpectedly did not show any improvement.
 However when SMN1 was returned to other motor circuit neurons - in particular, proprioceptive neurons and interneurons – the muscle size and motor function were restored. The proprioceptive neurons in motor circuits pick up and relay information to the spinal cord and brain about the body's position in space, which is then processed in the CNS and relayed via interneurons back to the motor neurons to stimulate muscle movement.
However when SMN1 was returned to other motor circuit neurons - in particular, proprioceptive neurons and interneurons – the muscle size and motor function were restored. The proprioceptive neurons in motor circuits pick up and relay information to the spinal cord and brain about the body's position in space, which is then processed in the CNS and relayed via interneurons back to the motor neurons to stimulate muscle movement.
In another experiment the researchers demonstrated that in fruit flies with defective SMN1, proprioceptive neurons and interneurons do not produce enough neurotransmitters. The muscle size and motor function improved when the flies' potassium channels were genetically blocked thereby increasing neurotransmitter output. The same effect was seen when the flies were given drugs that block potassium channels, leading to suggestions that this class of drugs might help patients with SMA.
Supported by these findings, in July 2012, the SMA Clinical Research Center at CUMC launched a clinical trial of a potassium channel blocker called dalfampridine (Ampyra) for the treatment of patients with SMA.
The study will assess whether the Dalfampriine improves walking ability and endurance in adults with SMA Type 3, compared with placebo. Claudia A. Chiriboga, MD, MPH, associate professor of Clinical Neurology at CUMC, is the lead clinical investigator. Ampyra was approved by the FDA for the treatment of patients with multiple sclerosis in 2010.
In a second study2, led jointly by Livio Pellizzoni, PhD, assistant professor of Pathology and Cell Biology in the Motor Neuron Center, and Dr. McCabe looked at why even though mutations in the disease gene SMN1 results in reduced expression in all cells, its only the motor system that is affected in patients with SMA.
Working with models of SMA in mammalian cells, fruit flies, zebrafish, and mice, the researchers demonstrated that SMN1 deficiency disrupts a fundamental cellular process known as RNA splicing (removal of parts of RNA called introns so that a gene can be translated into protein) with detrimental effects on the expression of a subset of genes that contain a rare type of intron.
 By studying the function of this group of genes affected by the loss of SMN1, the researchers discovered a novel gene - which they named stasimon - that is critically required for motor circuit activity in vivo. They further showed that restoring expression of stasimon was alone sufficient to correct key aspects of motor dysfunction in both invertebrate and vertebrate models of SMA.
By studying the function of this group of genes affected by the loss of SMN1, the researchers discovered a novel gene - which they named stasimon - that is critically required for motor circuit activity in vivo. They further showed that restoring expression of stasimon was alone sufficient to correct key aspects of motor dysfunction in both invertebrate and vertebrate models of SMA.
The implication is that this gene and the pathway in which it functions might be new candidate therapeutic targets The loss of the SMN1 gene has been directly linked to defective splicing of a critical neuronal gene to motor circuit dysfunction. The study thus points to SMA being a disease of RNA splicing.
References:
Read More