Age at loss of ambulation in STRIDE Registry and CINRG Natural History Study patients with DMD: a matched cohort analysis
Eugenio Mercuri, Francesco Muntoni, Filippo Buccella, Isabelle Desguerre, Janbernd Kirschner, Andrés Nascimento Osorio, Már Tulinius, Shelley Johnson, Christian Werner, Joel Jiang, James Li, Panayiota Trifillis, Craig. M. McDonald
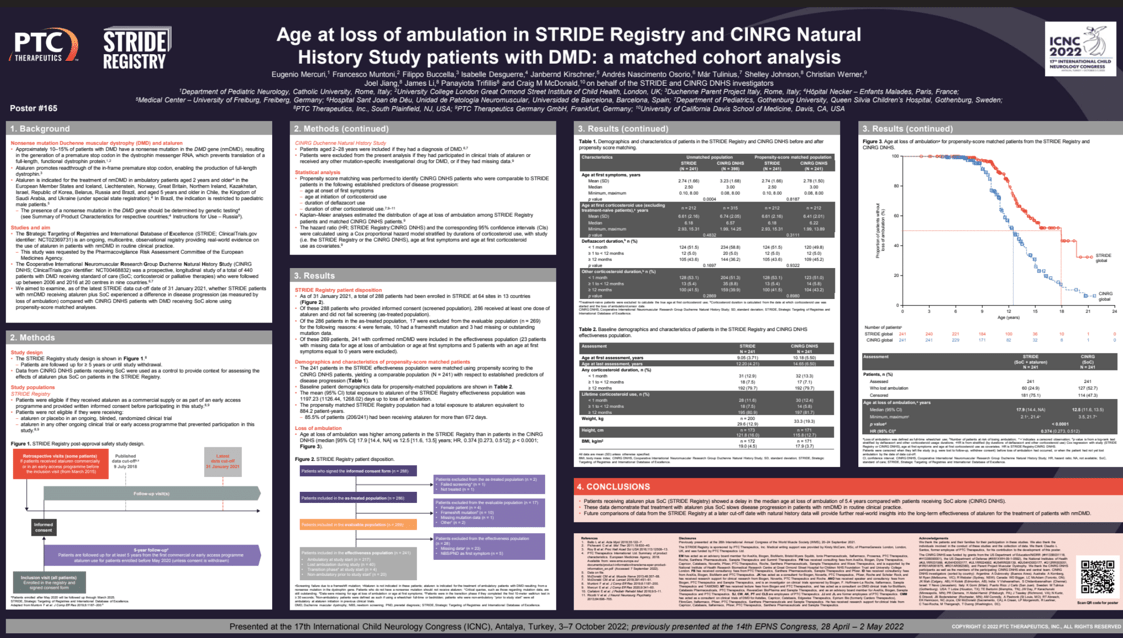
Objectives: We examined if nonsense mutation Duchenne muscular dystrophy (nmDMD) patients receiving ataluren plus standard of care (SoC) in the Strategic Targeting of Registries and International Database of Excellence (STRIDE) Registry (NCT02369731) experienced delayed loss of ambulation (LoA) versus DMD patients receiving SoC alone in the Cooperative International Neuromuscular Research Group (CINRG) Duchenne Natural History Study (NCT00468832).
Methods: STRIDE is an ongoing, multicenter, observational registry providing data on ataluren use in nmDMD patients in routine clinical practice (data extracted, January 31, 2021). Propensity score matching identified STRIDE and CINRG patient cohorts (N=241) comparable in established predictors of disease progression: age at first symptoms and initiation of corticosteroids, and duration of deflazacort and other corticosteroid use. Patients from CINRG who received DMD investigational drugs were excluded. Kaplan–Meier analyses were used to estimate age at LOA.
Results: Mean (SD) ages at first symptoms in the STRIDE and CINRG cohorts (N=241 per cohort) were 2.7 (1.7) and 2.8 (1.5) years, respectively. Most patients (STRIDE vs CINRG) received corticosteroids for ≥12 months (79.7% per cohort); similar proportions received deflazacort (43.6% vs 45.2%) or other corticosteroids (41.5% vs 43.2%). In STRIDE, 24.9% (60/241) of patients lost ambulation versus 52.7% (127/241) of CINRG patients. The median (95% CI) ages at LoA (STRIDE vs CINRG) were 17.9 (14.4, non-estimable) and 12.5 (11.6, 13.5) years, respectively. Ataluren plus SoC delayed age at LoA compared with SoC alone (p<0.0001).
Conclusion: These interim registry data show that ataluren treatment and SoC in routine clinical practice slows nmDMD disease progression.
Keywords: Duchenne muscular dystrophy; loss of ambulation; STRIDE.
Eugenio Mercuri
Catholic University
Italy
Francesco Muntoni
University College London Great Ormond Street Institute of Child Health
United Kingdom
Filippo Buccella
Parent Project APS
Italy
Isabelle Desguerre
Hôpital Necker – Enfants Malades
France
Janbernd Kirschner
Medical Center – University of Freiburg
Germany
Andrés Nascimento Osorio
Hospital Sant Joan de Déu, Unidad de Patología Neuromuscular, Universidad de Barcelona
Spain
Már Tulinius
Gothenburg University, Queen Silvia Children’s Hospital
Sweden
Shelley Johnson
PTC Therapeutics Inc.
United States
Christian Werner
PTC Therapeutics Germany GmbH
Germany
Joel Jiang
PTC Therapeutics Inc.
United States
James Li
PTC Therapeutics Inc.
United States
Panayiota Trifillis
PTC Therapeutics Inc.
United States
Craig. M. McDonald
University of California Davis School of Medicine
United States
Objectives: We examined if nonsense mutation Duchenne muscular dystrophy (nmDMD) patients receiving ataluren plus standard of care (SoC) in the Strategic Targeting of Registries and International Database of Excellence (STRIDE) Registry (NCT02369731) experienced delayed loss of ambulation (LoA) versus DMD patients receiving SoC alone in the Cooperative International Neuromuscular Research Group (CINRG) Duchenne Natural History Study (NCT00468832).
Methods: STRIDE is an ongoing, multicenter, observational registry providing data on ataluren use in nmDMD patients in routine clinical practice (data extracted, January 31, 2021). Propensity score matching identified STRIDE and CINRG patient cohorts (N=241) comparable in established predictors of disease progression: age at first symptoms and initiation of corticosteroids, and duration of deflazacort and other corticosteroid use. Patients from CINRG who received DMD investigational drugs were excluded. Kaplan–Meier analyses were used to estimate age at LOA.
Results: Mean (SD) ages at first symptoms in the STRIDE and CINRG cohorts (N=241 per cohort) were 2.7 (1.7) and 2.8 (1.5) years, respectively. Most patients (STRIDE vs CINRG) received corticosteroids for ≥12 months (79.7% per cohort); similar proportions received deflazacort (43.6% vs 45.2%) or other corticosteroids (41.5% vs 43.2%). In STRIDE, 24.9% (60/241) of patients lost ambulation versus 52.7% (127/241) of CINRG patients. The median (95% CI) ages at LoA (STRIDE vs CINRG) were 17.9 (14.4, non-estimable) and 12.5 (11.6, 13.5) years, respectively. Ataluren plus SoC delayed age at LoA compared with SoC alone (p<0.0001).
Conclusion: These interim registry data show that ataluren treatment and SoC in routine clinical practice slows nmDMD disease progression.
Keywords: Duchenne muscular dystrophy; loss of ambulation; STRIDE.
Eugenio Mercuri
Catholic University
Italy
Francesco Muntoni
University College London Great Ormond Street Institute of Child Health
United Kingdom
Filippo Buccella
Parent Project APS
Italy
Isabelle Desguerre
Hôpital Necker – Enfants Malades
France
Janbernd Kirschner
Medical Center – University of Freiburg
Germany
Andrés Nascimento Osorio
Hospital Sant Joan de Déu, Unidad de Patología Neuromuscular, Universidad de Barcelona
Spain
Már Tulinius
Gothenburg University, Queen Silvia Children’s Hospital
Sweden
Shelley Johnson
PTC Therapeutics Inc.
United States
Christian Werner
PTC Therapeutics Germany GmbH
Germany
Joel Jiang
PTC Therapeutics Inc.
United States
James Li
PTC Therapeutics Inc.
United States
Panayiota Trifillis
PTC Therapeutics Inc.
United States
Craig. M. McDonald
University of California Davis School of Medicine
United States