To determine the prevalence of comorbidities among children with cerebral palsy (CP) and risk-factors predictive of different comorbidities.
Ruchika Jha, Maya Vishwanath, Ankita Dilip Gambhirao, Arjun Kurup, Sachendra Badal, Sarvesh Kohli, Parvathi Parappil, Biju M John, Krishna Moorthy Adhikari, Vishal Sondhi
Objectives To determine the prevalence of comorbidities among children with cerebral palsy (CP) and risk-factors predictive of different comorbidities.
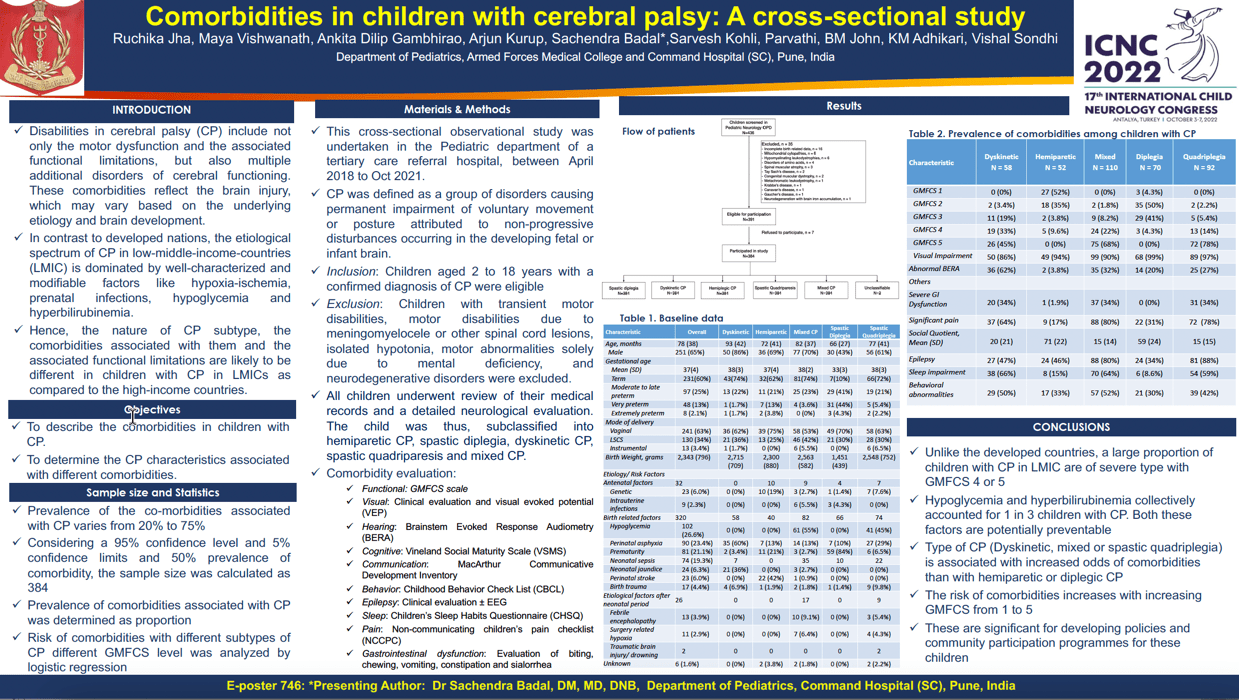
Methods Children aged 2-18 years with a confirmed diagnosis of CP were enrolled in this cross-sectional study undertaken between April 2018 and October 2021 at a tertiary care centre in India. Comorbidities were assessed in the following domains: motor function, cognition, vision, hearing, communication, epilepsy, sleep, pain, gastrointestinal dysfunction, and behaviour.
Results Among 436 children who were screened, 384 were study-eligible (Figure 1) and included mixed CP (110, 28.6%), spastic quadriparesis (92, 24%), spastic diplegia (70, 18.2%), dyskinetic CP (58, 15.1%), and hemiparetic CP (52, 13.5%) (Table 1). The most common comorbidities included visual impairment (357, 93%), epilepsy (245, 64%), impaired cognition (241, 62.7%), poor functional status (239, 62.2%), sleep impairment (176, 60.7%), pain (230, 60%), gastrointestinal dysfunction (224, 58.3%), language impairments (178, 46%) and behavioural abnormalities (165, 43%) (Table 2). As compared to hemiparetic CP, the odds (95% CI) of visual impairment, hearing impairment, communication abnormality, epilepsy, gastrointestinal dysfunction, pain, sleep impairment, and internalizing behaviour in a child with spastic quadriparesis were 1.82 (0.33-10.1), 9.47 (2.65-60.6), 98.7 (33.3-357), 8.59 (3.83-20.5), 2.77 (1.08-7.30), 15.6 (6.74-39.5), 14.0 (5.41-40.1), and 4.49 (1.85-12.7). Overall, the prevalence and severity of comorbidities were worst for spastic quadriparesis and mixed CP and worsened with increasing GMFCS scales (Table 3).
Conclusion These findings demonstrate a high prevalence of comorbidities beyond the functional domains, among children with CP. Identifying these is imperative for holistic care of children with CP.
Keywords: Cerebral Palsy
Ruchika Jha
AFMC
India
Maya Vishwanath
AFMC
India
Ankita Dilip Gambhirao
AFMC
India
Arjun Kurup
AFMC
India
Sachendra Badal
AFMC
India
Sarvesh Kohli
AFMC
India
Parvathi Parappil
AFMC
India
Biju M John
AFMC
India
Krishna Moorthy Adhikari
AFMC
India
Vishal Sondhi
AFMC
India
Objectives To determine the prevalence of comorbidities among children with cerebral palsy (CP) and risk-factors predictive of different comorbidities.
Methods Children aged 2-18 years with a confirmed diagnosis of CP were enrolled in this cross-sectional study undertaken between April 2018 and October 2021 at a tertiary care centre in India. Comorbidities were assessed in the following domains: motor function, cognition, vision, hearing, communication, epilepsy, sleep, pain, gastrointestinal dysfunction, and behaviour.
Results Among 436 children who were screened, 384 were study-eligible (Figure 1) and included mixed CP (110, 28.6%), spastic quadriparesis (92, 24%), spastic diplegia (70, 18.2%), dyskinetic CP (58, 15.1%), and hemiparetic CP (52, 13.5%) (Table 1). The most common comorbidities included visual impairment (357, 93%), epilepsy (245, 64%), impaired cognition (241, 62.7%), poor functional status (239, 62.2%), sleep impairment (176, 60.7%), pain (230, 60%), gastrointestinal dysfunction (224, 58.3%), language impairments (178, 46%) and behavioural abnormalities (165, 43%) (Table 2). As compared to hemiparetic CP, the odds (95% CI) of visual impairment, hearing impairment, communication abnormality, epilepsy, gastrointestinal dysfunction, pain, sleep impairment, and internalizing behaviour in a child with spastic quadriparesis were 1.82 (0.33-10.1), 9.47 (2.65-60.6), 98.7 (33.3-357), 8.59 (3.83-20.5), 2.77 (1.08-7.30), 15.6 (6.74-39.5), 14.0 (5.41-40.1), and 4.49 (1.85-12.7). Overall, the prevalence and severity of comorbidities were worst for spastic quadriparesis and mixed CP and worsened with increasing GMFCS scales (Table 3).
Conclusion These findings demonstrate a high prevalence of comorbidities beyond the functional domains, among children with CP. Identifying these is imperative for holistic care of children with CP.
Keywords: Cerebral Palsy
Ruchika Jha
AFMC
India
Maya Vishwanath
AFMC
India
Ankita Dilip Gambhirao
AFMC
India
Arjun Kurup
AFMC
India
Sachendra Badal
AFMC
India
Sarvesh Kohli
AFMC
India
Parvathi Parappil
AFMC
India
Biju M John
AFMC
India
Krishna Moorthy Adhikari
AFMC
India
Vishal Sondhi
AFMC
India
Ruchika Jha
AFMC
India
India