Pathogenesis of nodding syndrome; Preliminary findings
Richard Idro, Maria Pia Giannocaro, Angela Vincent
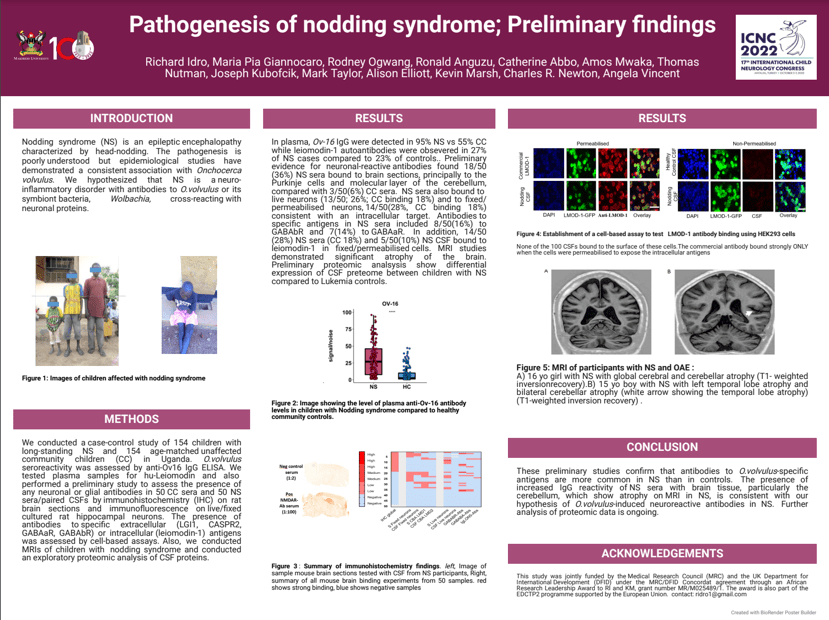
Objective Nodding syndrome (NS) is an epileptic encephalopathy characterized by head-nodding. The pathogenesis is poorly understood but epidemiological studies have demonstrated a consistent association with Onchocerca volvulus. We hypothesized NS is a neuro-inflammatory disorder with antibodies to O.volvulus or its symbiont bacteria, Wolbachia, cross-reacting with neuronal proteins.
Method: We conducted a case-control study of 154 children with long-standing NS and 154 age-matched unaffected children (CC) in Uganda. O.volvulus seroreactivity was assessed by anti-Ov16 IgG. We also conducted a preliminary study of neuronal/glial antibodies in 50 CC-sera and 50 NS-sera/paired CSFs by immunohistochemistry on rat brain sections and immunofluorescence on cultured rat hippocampal neurons. The presence of antibodies to extracellular (LGI1, CASPR2, GABAaR, GABAbR) or intracellular (leiomodin-1) antigens was assessed by cell-based assays.
Result: Ov-16 IgG were detected in 95% NS vs 55% CC. Neuronal-reactive antibodies were found in 18/50(36%) NS sera bound principally to the Purkinje cells and the molecular layer of cerebellum, compared with 3/50(6%) CC sera. NS sera also bound to live neurons and to fixed/permeabilized neurons consistent with an intracellular target. Antibodies to specific antigens in NS sera included 8/50(16%) to GABAbR and 7(14%) GABAaR. In addition, 14/50(28%) NS sera (CC 18%) and 5/50(10%) NS CSF-bound to leiomodin-1 in fixed/permeabilised cells.
Conclusions: Antibodies to O.volvulus-specific antigens are more common in NS vs controls. Increased reactivity of NS sera with brain tissue is consistent with our hypothesis of O.volvulus-induced neuroreactive antibodies in NS. Furthermore, IgG reactivity of NS CSF with leiomodin-1 would support its use as NS biomarker.
Keywords: Nodding syndrome, pathogenesis
Richard Idro
Mulago hospital and Makerere University College of Health Sciences
Uganda
Maria Pia Giannocaro
University of Bologna, IRCCS Istituto delle Scienze Neurologiche di Bologna, UOC Clinica Neurologica
Italy
Angela Vincent
University of Oxford
United Kingdom
Objective Nodding syndrome (NS) is an epileptic encephalopathy characterized by head-nodding. The pathogenesis is poorly understood but epidemiological studies have demonstrated a consistent association with Onchocerca volvulus. We hypothesized NS is a neuro-inflammatory disorder with antibodies to O.volvulus or its symbiont bacteria, Wolbachia, cross-reacting with neuronal proteins.
Method: We conducted a case-control study of 154 children with long-standing NS and 154 age-matched unaffected children (CC) in Uganda. O.volvulus seroreactivity was assessed by anti-Ov16 IgG. We also conducted a preliminary study of neuronal/glial antibodies in 50 CC-sera and 50 NS-sera/paired CSFs by immunohistochemistry on rat brain sections and immunofluorescence on cultured rat hippocampal neurons. The presence of antibodies to extracellular (LGI1, CASPR2, GABAaR, GABAbR) or intracellular (leiomodin-1) antigens was assessed by cell-based assays.
Result: Ov-16 IgG were detected in 95% NS vs 55% CC. Neuronal-reactive antibodies were found in 18/50(36%) NS sera bound principally to the Purkinje cells and the molecular layer of cerebellum, compared with 3/50(6%) CC sera. NS sera also bound to live neurons and to fixed/permeabilized neurons consistent with an intracellular target. Antibodies to specific antigens in NS sera included 8/50(16%) to GABAbR and 7(14%) GABAaR. In addition, 14/50(28%) NS sera (CC 18%) and 5/50(10%) NS CSF-bound to leiomodin-1 in fixed/permeabilised cells.
Conclusions: Antibodies to O.volvulus-specific antigens are more common in NS vs controls. Increased reactivity of NS sera with brain tissue is consistent with our hypothesis of O.volvulus-induced neuroreactive antibodies in NS. Furthermore, IgG reactivity of NS CSF with leiomodin-1 would support its use as NS biomarker.
Keywords: Nodding syndrome, pathogenesis
Richard Idro
Mulago hospital and Makerere University College of Health Sciences
Uganda
Maria Pia Giannocaro
University of Bologna, IRCCS Istituto delle Scienze Neurologiche di Bologna, UOC Clinica Neurologica
Italy
Angela Vincent
University of Oxford
United Kingdom
Richard Idro
Mulago hospital and Makerere University College of Health Sciences Uganda
Mulago hospital and Makerere University College of Health Sciences Uganda