High Diagnostic Yield Of Non-Contrast Brain MRI With SWI In Non-Sedated Children With Sturge-Weber Syndrome
Introduction: Pre-/post-contrast MRI obtained under anesthesia is used to evaluate and follow brain abnormalities in children with Sturge-Weber syndrome (SWS). However, anesthesia and contrast administration carry risks. We explored the feasibility and diagnostic utility of a safe non-contrast, non-sedate MRI acquisition with susceptibility-weighted imaging [SWI] in SWS children and their siblings with a wide range of cognitive and behavioral functioning.
Methods: Thirty children (15 with SWS, 15 siblings; mean age: 11.8 and 11.1 years, respectively) underwent a non-sedate 15-minute native brain MRI (3T) acquisition (SWI, T1, T2, fluid-attenuated inversion recovery) and formal neurocognitive and behavioral assessment, prospectively. Children were given extra time in the scanner, and young children were scanned in natural sleep. MRI abnormalities in the SWS group were compared to those identified on previous clinical pre-/post-contrast MRI obtained with anesthesia.
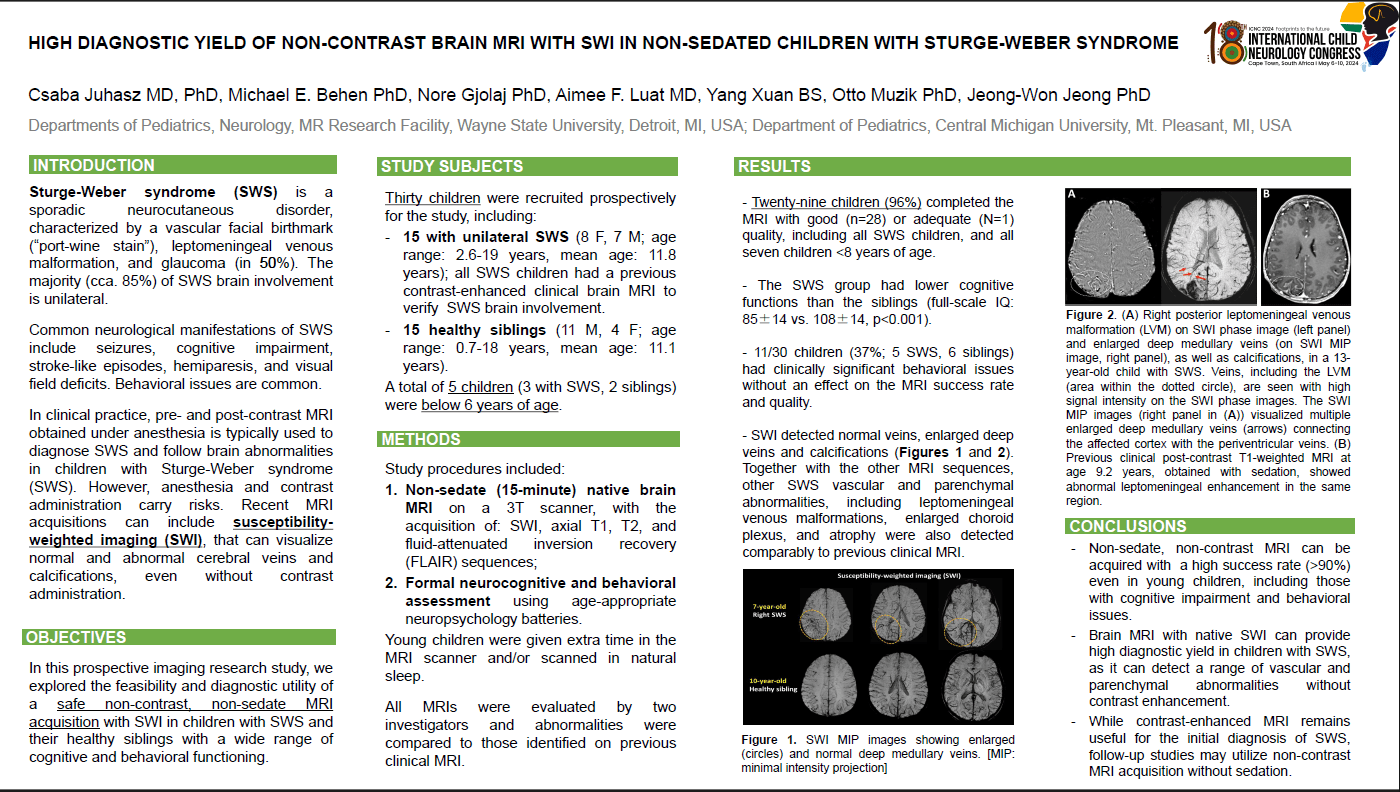
Results: Twenty-nine children (96%) completed the MRI with good (n=28) or adequate quality, including all SWS children, and all seven children <8 years of age. The SWS group had lower cognitive functions than the siblings (full-scale IQ: 85±14 vs. 108±14, p<0.001) and 11/30 children (37%; 5 SWS, 6 siblings) had clinically significant behavioral issues without an effect on the MRI success rate and quality. SWI detected both normal veins and SWS vascular abnormalities and calcifications (Figure) and, together with the other sequences, detected vascular and parenchymal abnormalities similar to or better than contrast-enhanced MRI.
Conclusion: Non-sedate, non-contrast MRI acquisition with SWI can provide high diagnostic yield in children with SWS, including those with cognitive impairment and/or behavioral concerns.
Csaba Juhasz
Professor
Pediatrics and Neurology
Wayne State University
Detroit, United States
Michael Behen
Assistant Professor
Pediatrics and Neurology
Wayne State University
Detroit, United States
Nore Gjolaj
Research ssistant
Pediatrics and Neurology
Wayne State University
Detroit, United States
Aimee Luat
Associate Professor
Pediatrics
Central Michigan University
Mt. Pleasant, United States
Yang Xuan
Research Assistant
MR Research Facility
Wayne State University
Detroit, United States
Otto Muzik
Professor
Pediatrics and Neurology
Wayne State University
Detroit, United States
Jeong-Won Jeong
Professor
Pediatrics and Neurology
Wayne State University
Detroit, United States