: An Unusual Case Presentation Of Graft Versus Host Myositis Secondary To Bone Marrow Transplant In A Toddler
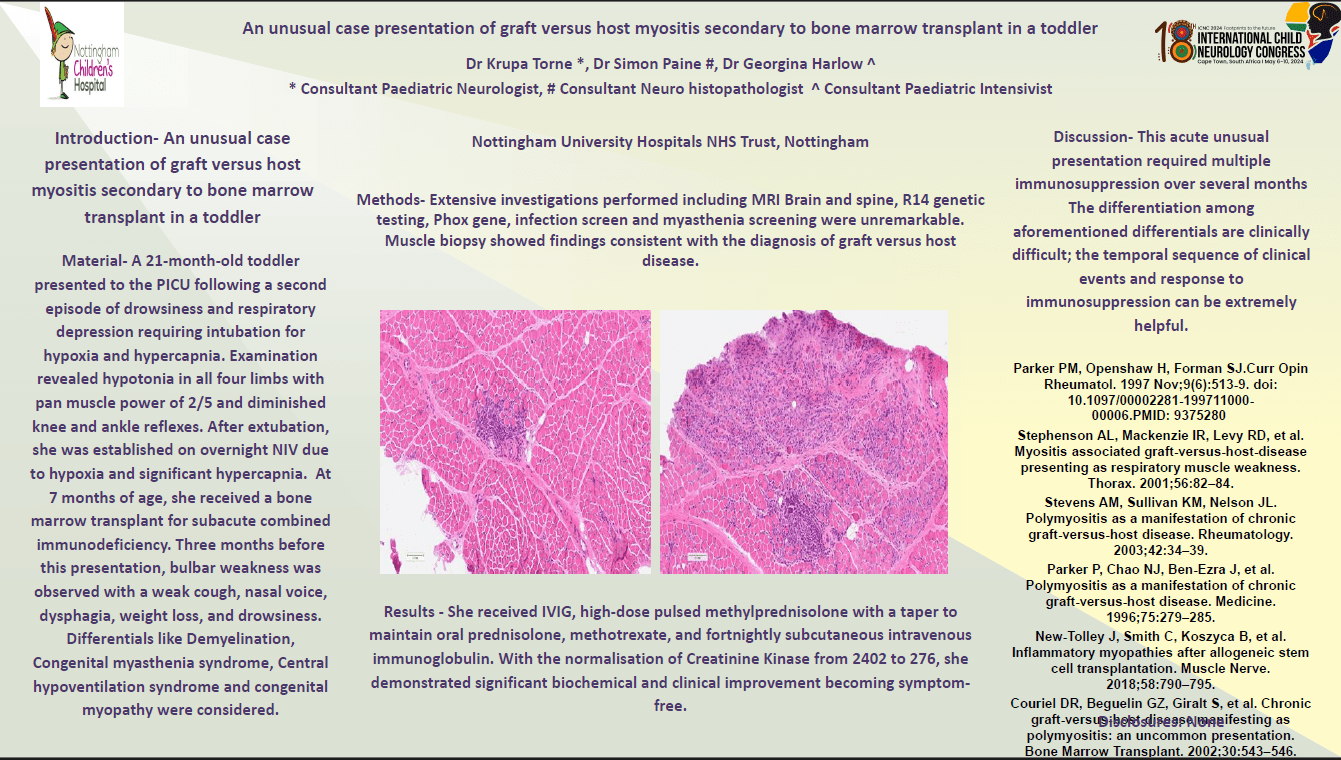
Introduction – Toddler with graft versus host myositis secondary to bone marrow transplant successfully treated with immunosuppression. Material- 21-month old toddler presented to PICU following second episode of drowsiness and respiratory depression requiring intubation for hypoxia and hypercapnia. Examination revealed hypotonia in all four limbs with pan muscle power of 2/5, diminished all reflexes. After extubation, was established on overnight NIV due to hypoxia and significant hypercapnia. At seven months of age, received bone marrow transplant for subacute combined immunodeficiency. Three months before this presentation, bulbar weakness was observed with weak cough, nasal voice, dysphagia, weight loss, and drowsiness. Differentials like Demyelination, Congenital myasthenia syndrome, Central hypoventilation syndrome and congenital myopathy considered. Methods-MRI Brain and spine, R14 genetic testing, Phox gene, infection screen and myasthenia screening unremarkable. Muscle biopsy showed findings consistent with the diagnosis of graft versus host disease. Results - Received IVIG, high-dose pulsed methylprednisolone with taper to maintain oral prednisolone, methotrexate, and fortnightly subcutaneous intravenous immunoglobulin. With normalisation of Creatinine Kinase from 2402 to 276, she demonstrated significant biochemical, clinical improvement becoming symptom-free. Discussion- This acute unusual presentation required multiple immunosuppression over several months The differentiation among aforementioned differentials is clinically difficult. Temporal sequence of clinical events and response to immunosuppression can be extremely helpful. Conclusion- Clinical presentation consistent with diagnosing graft versus host myositis secondary to bone marrow transplant based on clinical and histopathological evidence. To prevent unnecessary investigations and secondary complications, it is crucial to have high level of suspicion and precise diagnosis. Disclosures: None
Krupa Torne
Nottingham University Hospitals NHS Trust
United Kingdom
Simon Paine
Nottingham University Hospitals NHS Trust
United Kingdom
Georgina Harlow
Nottingham University Hospitals NHS Trust
United Kingdom