Clinical spectrum, treatment response and outcomes in children with Febrile Infection Related Epilepsy Syndrome (FIRES) : A case series from India
Ramya Bandi, Lokesh Lingappa, Vivek Jain, Ravi Sharma, Ramesh Konanki
Objectives : To study clinical profile, treatment and outcomes of children with Febrile infection related epilepsy syndrome (FIRES) from India
Methods: Multicentric, retrospective, descriptive study between July 2015-November 2020, in children aged 2-18 years, fulfilling the definition of FIRES.
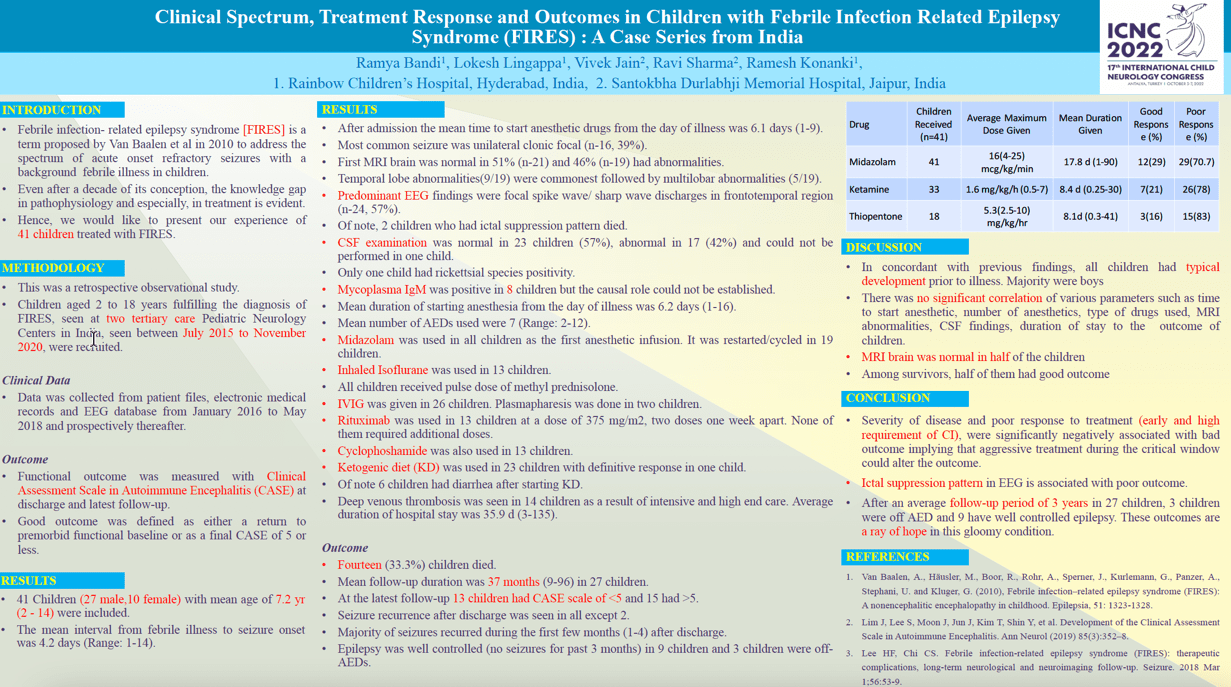
Results: 41 children included: 27 were boys, median age at onset was 7.2 years (Range: 2-14). Mean interval from febrile illness to seizure onset was 4.2 days (Range: 1-14). Mean time to start anaesthetic drug from day of illness was 6.1days (1-9). Most common seizure was unilateral clonic focal (n-16, 39%). First MRI brain was normal in 52% (n-22) and 26% (n-11) had abnormalities (temporal lobe changes). Commonest predominant EEG discharges were frontotemporal (n-24, 57%). CSF examination was normal in 23 children (56%). Mean number of AEDs used were 7 (Range: 2-12). Pharmacological Coma was used in all 42 children: Midazolam (N-42, Maximum dose (MD):16.2mcg/kg/min), Ketamine (n-33; MD:1.6mg/kg/hr), Thiopentone (n-19,5; MD: 5.3 mg/kg/hr) were the commonest agents. Inhaled Isoflurane (n-11) and Propofol infusion (n-1) were also used. Use of immunomodulation (Rituximab and/or Cyclophosphamide) was significantly associated with good outcome (CASE < 5). Fourteen (33.3%) children died. Mean follow-up duration was 37 months (9-96). Thirteen children had CASE scale of <5 and 15 had >5. Epilepsy was well controlled in 9 children and 3 children were off-AEDs.
Conclusion: Severity of disease and poor response to treatment (early and high requirement of anaesthetic infusion), were negatively associated with outcome, and aggressive treatment of FIRES during the critical window could alter the outcome.
Keywords: Epilepsy, FIRES, Status epilepticus, Anaesthetics
Ramya Bandi
Rainbow Children's Hospital, Hyderabad, India
India
Lokesh Lingappa
Rainbow Children's Hospital, Hyderabad, India
India
Vivek Jain
Santokbha Durlabhji Memorial Hospital, Jaipur, India
India
Ravi Sharma
Santokbha Durlabhji Memorial Hospital, Jaipur, India
India
Ramesh Konanki
Rainbow Children's Hospital, Hyderabad, India
India
Objectives : To study clinical profile, treatment and outcomes of children with Febrile infection related epilepsy syndrome (FIRES) from India
Methods: Multicentric, retrospective, descriptive study between July 2015-November 2020, in children aged 2-18 years, fulfilling the definition of FIRES.
Results: 41 children included: 27 were boys, median age at onset was 7.2 years (Range: 2-14). Mean interval from febrile illness to seizure onset was 4.2 days (Range: 1-14). Mean time to start anaesthetic drug from day of illness was 6.1days (1-9). Most common seizure was unilateral clonic focal (n-16, 39%). First MRI brain was normal in 52% (n-22) and 26% (n-11) had abnormalities (temporal lobe changes). Commonest predominant EEG discharges were frontotemporal (n-24, 57%). CSF examination was normal in 23 children (56%). Mean number of AEDs used were 7 (Range: 2-12). Pharmacological Coma was used in all 42 children: Midazolam (N-42, Maximum dose (MD):16.2mcg/kg/min), Ketamine (n-33; MD:1.6mg/kg/hr), Thiopentone (n-19,5; MD: 5.3 mg/kg/hr) were the commonest agents. Inhaled Isoflurane (n-11) and Propofol infusion (n-1) were also used. Use of immunomodulation (Rituximab and/or Cyclophosphamide) was significantly associated with good outcome (CASE < 5). Fourteen (33.3%) children died. Mean follow-up duration was 37 months (9-96). Thirteen children had CASE scale of <5 and 15 had >5. Epilepsy was well controlled in 9 children and 3 children were off-AEDs.
Conclusion: Severity of disease and poor response to treatment (early and high requirement of anaesthetic infusion), were negatively associated with outcome, and aggressive treatment of FIRES during the critical window could alter the outcome.
Keywords: Epilepsy, FIRES, Status epilepticus, Anaesthetics
Ramya Bandi
Rainbow Children's Hospital, Hyderabad, India
India
Lokesh Lingappa
Rainbow Children's Hospital, Hyderabad, India
India
Vivek Jain
Santokbha Durlabhji Memorial Hospital, Jaipur, India
India
Ravi Sharma
Santokbha Durlabhji Memorial Hospital, Jaipur, India
India
Ramesh Konanki
Rainbow Children's Hospital, Hyderabad, India
India
Ramya Bandi
Rainbow Children's Hospital, Hyderabad, India India
Rainbow Children's Hospital, Hyderabad, India India