A rare dual pathology: Idiopathic intracranial hypertension presenting with isolated unilateral facial nerve palsy
Aysen Gok, Dondu Ulker Ustebay, Semra Hız Kurul, Uluc Yis
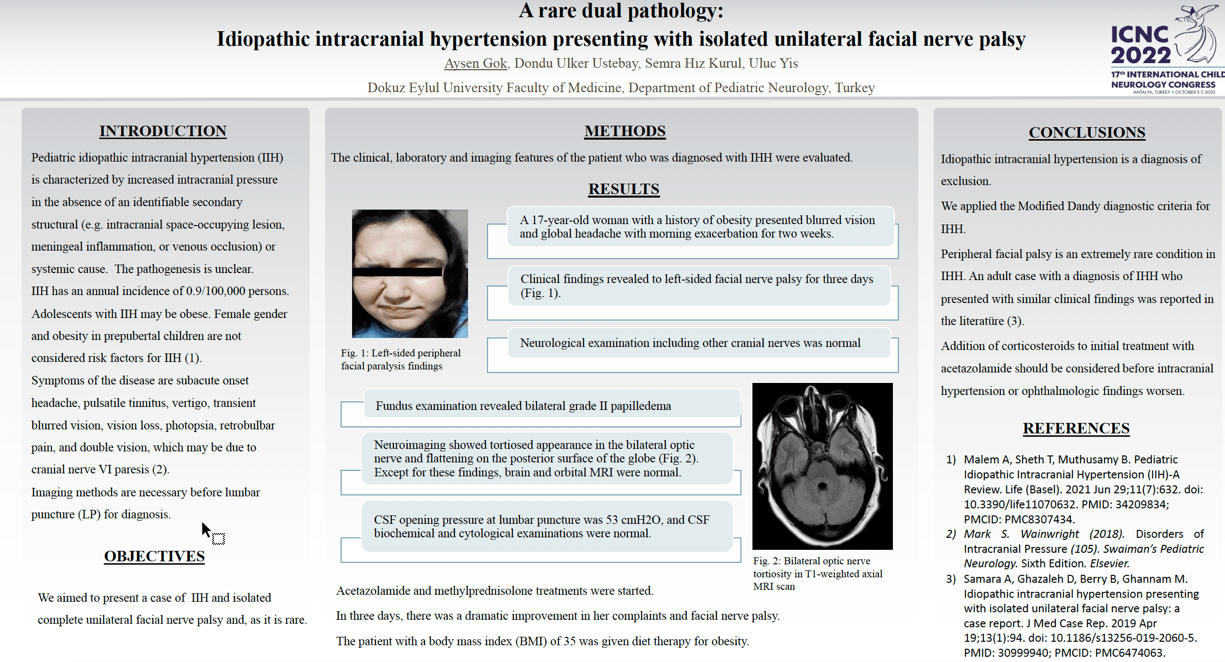
Objective: We aimed to present the association of idiopathic intracranial hypertension (IIH) and peripheral facial nerve palsy in a pediatric patient followed up in our clinic. Method: The clinical, laboratory and imaging characteristics of the patient diagnosed with idiopathic intracranial hypertension were examined. Results: A 17-year-old female patient with a history of obesity was admitted with complaints of headache and blurred vision that started two weeks ago. She had findings related to left-sided facial nerve palsy that started three days ago. Neurological examination including other cranial nerves was normal. Fundus examination revealed bilateral grade III papilledema. Neuroimaging was normal, except for the findings of a tortuous appearance in the bilateral optic nerves and flattening on the posterior surface of the globe. CSF opening pressure at lumbar puncture was 53 cmH2O, and CSF biochemical and cytological examinations were normal. The diagnosis of IIH was made according to the Modified Dandy Criteria. Acetazolamide and methylprednisolone treatments were started. In three days, there was a dramatic improvement in her complaints and facial nerve palsy. A diet with appropriate calories was arranged for her obesity. Conclusion: Idiopathic intracranial hypertension is a diagnosis of exclusion. Peripheral facial palsy is an extremely rare condition in IHH. Addition of corticosteroids to initial treatment with acetazolamide should be considered before intracranial hypertension or ophthalmologic findings worsen.
Keywords: IIH, peripheral, facial nerve palsy, papilledema
Aysen Gok
Turkey
Dondu Ulker Ustebay
Turkey
Semra Hız Kurul
Turkey
Uluc Yis
Turkey
Objective: We aimed to present the association of idiopathic intracranial hypertension (IIH) and peripheral facial nerve palsy in a pediatric patient followed up in our clinic. Method: The clinical, laboratory and imaging characteristics of the patient diagnosed with idiopathic intracranial hypertension were examined. Results: A 17-year-old female patient with a history of obesity was admitted with complaints of headache and blurred vision that started two weeks ago. She had findings related to left-sided facial nerve palsy that started three days ago. Neurological examination including other cranial nerves was normal. Fundus examination revealed bilateral grade III papilledema. Neuroimaging was normal, except for the findings of a tortuous appearance in the bilateral optic nerves and flattening on the posterior surface of the globe. CSF opening pressure at lumbar puncture was 53 cmH2O, and CSF biochemical and cytological examinations were normal. The diagnosis of IIH was made according to the Modified Dandy Criteria. Acetazolamide and methylprednisolone treatments were started. In three days, there was a dramatic improvement in her complaints and facial nerve palsy. A diet with appropriate calories was arranged for her obesity. Conclusion: Idiopathic intracranial hypertension is a diagnosis of exclusion. Peripheral facial palsy is an extremely rare condition in IHH. Addition of corticosteroids to initial treatment with acetazolamide should be considered before intracranial hypertension or ophthalmologic findings worsen.
Keywords: IIH, peripheral, facial nerve palsy, papilledema
Aysen Gok
Turkey
Dondu Ulker Ustebay
Turkey
Semra Hız Kurul
Turkey
Uluc Yis
Turkey
Aysen Gok
Turkey
Turkey