Neurocognitive Functions and Behavior Outcome of Preschool-Age Children with a History of Febrile Convulsions
Nuran Gozpinar, Bilgihan Bikmazer, Oguzhan Koyuncu, Aygun Hüseynova, Ferit Durankus, Elif Yuksel Karatoprak, Emek Uyur Yalcin, Nilufer Eldes Hacifazlioglu, Alperen Bikmazer, Vahdet Gormez
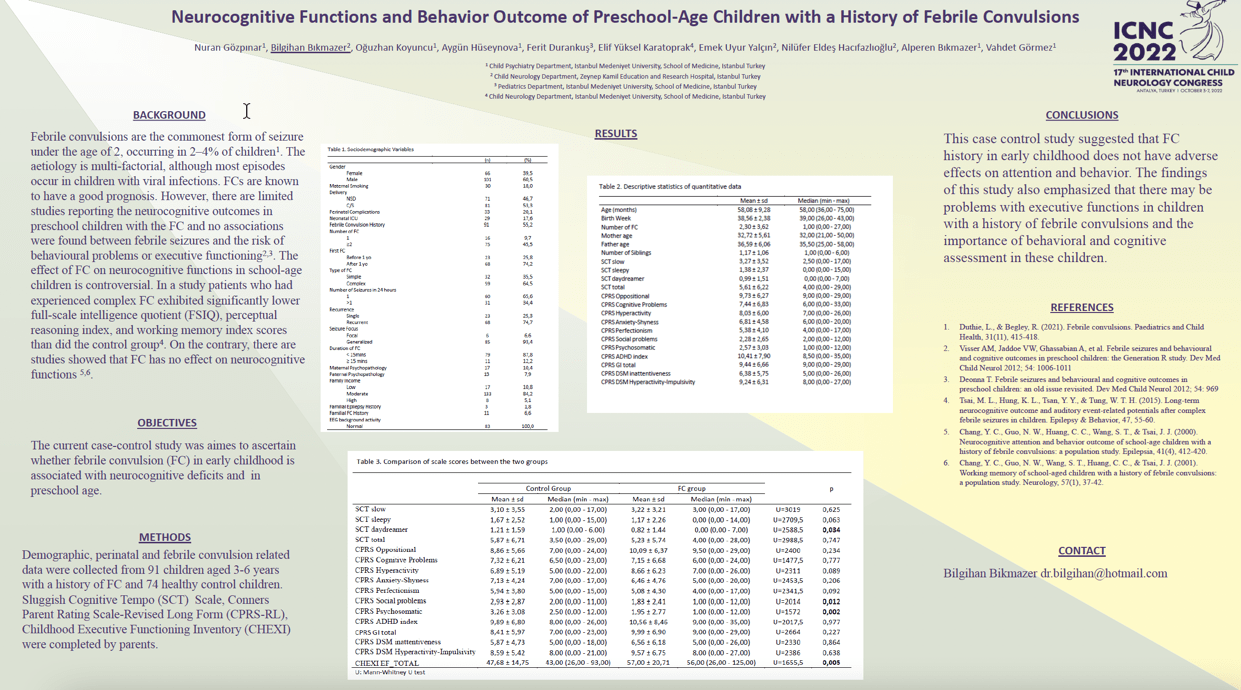
Objectives: The current case-control study was aimed to ascertain whether febrile convulsion (FC) is associated with neurocognitive deficits in preschool and school age children.
Methods: Demographic, perinatal and febrile convulsion related data of 91 children aged 3-6 years with a history of FC and 74 healthy control children were retrospectively collected. Sluggish Cognitive Tempo (SCT) Scale, Conners Parent Rating Scale-Revised Long Form (CPRS-RL), Childhood Executive Functioning Inventory (CHEXI) were completed by parents.
Results: There was no significant difference between slow, sleepy and total scores of the SCT scale and defiant, cognitive problems-inattentiveness, hyperactivity, anxiety and perfectionism subscale scores of CPRS-RL between the two groups. SCT daydreamer, CPRS-RL social problem and psychosomatic subscale scores were higher in the control group (p=0.034, p=0.012 and p=0.002, respectively). CHEXI Executive Functioning Total score was higher in the FC group (p=0.005).
Conclusion: This case control study suggested that FC history in early childhood does not have adverse effects on attention and behavior. The findings of this study also emphasized that there may be problems with executive functions in children with a history of febrile convulsions. Therefore, behavioral and cognitive assessment of children with FC is recommended.
Keywords: Febrile Convulsion, behaviour, Sluggish Cognitive Tempo
Nuran Gozpinar
Istanbul Medeniyet University School Of Medicine
Turkey
Bilgihan Bikmazer
Zeynep Kamil Obstetric and Pediatric Diseases Training and Research Hospital, The University of Health Sciences
Turkey
Oguzhan Koyuncu
Istanbul Medeniyet University School Of Medicine
Turkey
Aygun Hüseynova
Istanbul Medeniyet University School Of Medicine
Turkey
Ferit Durankus
Istanbul Medeniyet University School Of Medicine
Turkey
Elif Yuksel Karatoprak
Istanbul Medeniyet University School Of Medicine
Turkey
Emek Uyur Yalcin
Health Sciences University Zeynep Kamil Gynecology and Pediatrics Hospital
Turkey
Nilufer Eldes Hacifazlioglu
Health Sciences University Zeynep Kamil Gynecology and Pediatrics Hospital
Turkey
Alperen Bikmazer
Istanbul Medeniyet University School Of Medicine
Turkey
Vahdet Gormez
Istanbul Medeniyet University School Of Medicine
Turkey
Objectives: The current case-control study was aimed to ascertain whether febrile convulsion (FC) is associated with neurocognitive deficits in preschool and school age children.
Methods: Demographic, perinatal and febrile convulsion related data of 91 children aged 3-6 years with a history of FC and 74 healthy control children were retrospectively collected. Sluggish Cognitive Tempo (SCT) Scale, Conners Parent Rating Scale-Revised Long Form (CPRS-RL), Childhood Executive Functioning Inventory (CHEXI) were completed by parents.
Results: There was no significant difference between slow, sleepy and total scores of the SCT scale and defiant, cognitive problems-inattentiveness, hyperactivity, anxiety and perfectionism subscale scores of CPRS-RL between the two groups. SCT daydreamer, CPRS-RL social problem and psychosomatic subscale scores were higher in the control group (p=0.034, p=0.012 and p=0.002, respectively). CHEXI Executive Functioning Total score was higher in the FC group (p=0.005).
Conclusion: This case control study suggested that FC history in early childhood does not have adverse effects on attention and behavior. The findings of this study also emphasized that there may be problems with executive functions in children with a history of febrile convulsions. Therefore, behavioral and cognitive assessment of children with FC is recommended.
Keywords: Febrile Convulsion, behaviour, Sluggish Cognitive Tempo
Nuran Gozpinar
Istanbul Medeniyet University School Of Medicine
Turkey
Bilgihan Bikmazer
Zeynep Kamil Obstetric and Pediatric Diseases Training and Research Hospital, The University of Health Sciences
Turkey
Oguzhan Koyuncu
Istanbul Medeniyet University School Of Medicine
Turkey
Aygun Hüseynova
Istanbul Medeniyet University School Of Medicine
Turkey
Ferit Durankus
Istanbul Medeniyet University School Of Medicine
Turkey
Elif Yuksel Karatoprak
Istanbul Medeniyet University School Of Medicine
Turkey
Emek Uyur Yalcin
Health Sciences University Zeynep Kamil Gynecology and Pediatrics Hospital
Turkey
Nilufer Eldes Hacifazlioglu
Health Sciences University Zeynep Kamil Gynecology and Pediatrics Hospital
Turkey
Alperen Bikmazer
Istanbul Medeniyet University School Of Medicine
Turkey
Vahdet Gormez
Istanbul Medeniyet University School Of Medicine
Turkey
Bilgihan Bikmazer
Zeynep Kamil Obstetric and Pediatric Diseases Training and Research Hospital, The University of Health Sciences Turkey
Zeynep Kamil Obstetric and Pediatric Diseases Training and Research Hospital, The University of Health Sciences Turkey