A retrospective study of central nervous system vasculitis patients
Sarolta Dobner, Zoltán Liptai, Léna Szabó, Tamás Constantin, Edit Varga, Benke Péter, Barsi Péter, Mária Anna Hudák
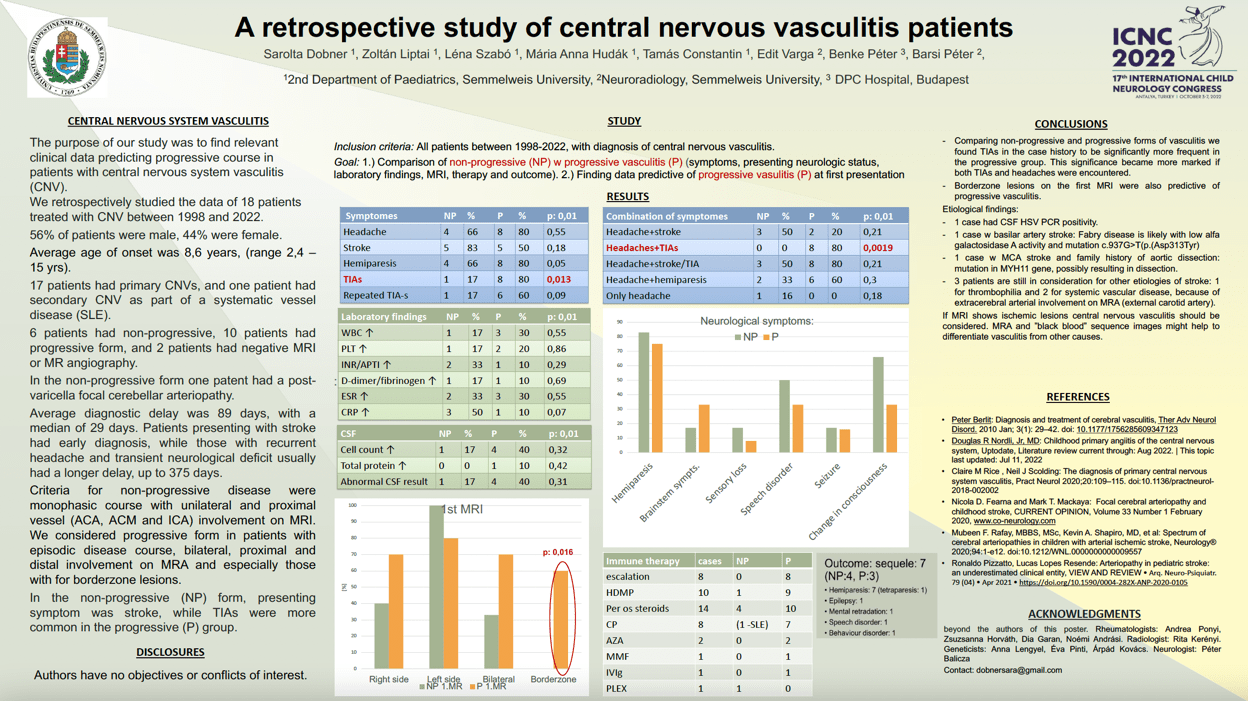
Objectives: The purpose of our study was to find relevant clinical data predicting progressive course in patients with central nervous system vasculitis (CNSV). Methods: A retrospective study of 15 patients treated with CNSV between 1998 and 2021. 60 % of patients were male. 12 patients had primary CNSV-s, one had postVZV CNSV, and two had systematic vessel disease. 33% showed nonprogressive (NP) course presenting with stroke, while TIA-s were more common in the progressive (P) group. We compared the two forms regarding presenting symptoms, laboratory, CSF results, serologic studies, autoantibodies, thrombophilia studies, MRIs and EEG findings, therapy and outcome were studied. Results: Average age of onset was 9 yrs in NP, and 8 yrs for P form. Delay of diagnosis was 82 days in the P and 44 days in the NP form. Most common presenting symptom was hemiparesis (73%) in both groups. MRA showed vessel involvement in all cases except for the one MRI negative case. Repeated MRAs were needed for progressive CNSV diagnosis in 9 cases, though 7 patients’ first MRAs already suggested the P from (distal, and bilateral involvement). Despite extended etiologic studies we found underlying trigger in only few cases. 80% of patients received immunotherapy, escalation was necessary in 60%. Sequelae were present in 40% of cases, most commonly hemiparesis. Conclusions: Predictors of developing progressive CNSV were headache, repeated TIA episodes, bilateral, proximal and distal vessel involvement on MRA, emphasizing the importance of the first MRA evaluation.
Keywords: vasculitis, progressive, non-progressive, bilateral, distal
Sarolta Dobner
2nd Department of Paediatrics, Semmelweis University
Hungary
Zoltán Liptai
2nd Department of Paediatrics, Semmelweis University
Hungary
Léna Szabó
2nd Department of Paediatrics, Semmelweis University
Hungary
Tamás Constantin
2nd Department of Paediatrics, Semmelweis University
Hungary
Edit Varga
Neuroradiology, Semmelweis University
Hungary
Benke Péter
DPC OHII Hospital Budapest
Hungary
Barsi Péter
Neuroradiology, Semmelweis University
Hungary
Mária Anna Hudák
2nd Department of Paediatrics, Semmelweis University
Hungary
Objectives: The purpose of our study was to find relevant clinical data predicting progressive course in patients with central nervous system vasculitis (CNSV). Methods: A retrospective study of 15 patients treated with CNSV between 1998 and 2021. 60 % of patients were male. 12 patients had primary CNSV-s, one had postVZV CNSV, and two had systematic vessel disease. 33% showed nonprogressive (NP) course presenting with stroke, while TIA-s were more common in the progressive (P) group. We compared the two forms regarding presenting symptoms, laboratory, CSF results, serologic studies, autoantibodies, thrombophilia studies, MRIs and EEG findings, therapy and outcome were studied. Results: Average age of onset was 9 yrs in NP, and 8 yrs for P form. Delay of diagnosis was 82 days in the P and 44 days in the NP form. Most common presenting symptom was hemiparesis (73%) in both groups. MRA showed vessel involvement in all cases except for the one MRI negative case. Repeated MRAs were needed for progressive CNSV diagnosis in 9 cases, though 7 patients’ first MRAs already suggested the P from (distal, and bilateral involvement). Despite extended etiologic studies we found underlying trigger in only few cases. 80% of patients received immunotherapy, escalation was necessary in 60%. Sequelae were present in 40% of cases, most commonly hemiparesis. Conclusions: Predictors of developing progressive CNSV were headache, repeated TIA episodes, bilateral, proximal and distal vessel involvement on MRA, emphasizing the importance of the first MRA evaluation.
Keywords: vasculitis, progressive, non-progressive, bilateral, distal
Sarolta Dobner
2nd Department of Paediatrics, Semmelweis University
Hungary
Zoltán Liptai
2nd Department of Paediatrics, Semmelweis University
Hungary
Léna Szabó
2nd Department of Paediatrics, Semmelweis University
Hungary
Tamás Constantin
2nd Department of Paediatrics, Semmelweis University
Hungary
Edit Varga
Neuroradiology, Semmelweis University
Hungary
Benke Péter
DPC OHII Hospital Budapest
Hungary
Barsi Péter
Neuroradiology, Semmelweis University
Hungary
Mária Anna Hudák
2nd Department of Paediatrics, Semmelweis University
Hungary
Sarolta Dobner
2nd Department of Paediatrics, Semmelweis University Hungary
2nd Department of Paediatrics, Semmelweis University Hungary