Clinical and molecular spectrum of tuberous sclerosis complex in a regional cohort: an efficacy and outcome study with antiseizure medication plus mTOR inhibitor therapy
Meltem Orbay, Hepsen Mine Serin, Seda Kanmaz, Esra Isik, Tahir Atik, Ozgur Cogulu, Ferda Ozkinay, Sanem Yılmaz, Gul Aktan, Sarenur Gökben, Hasan Tekgül
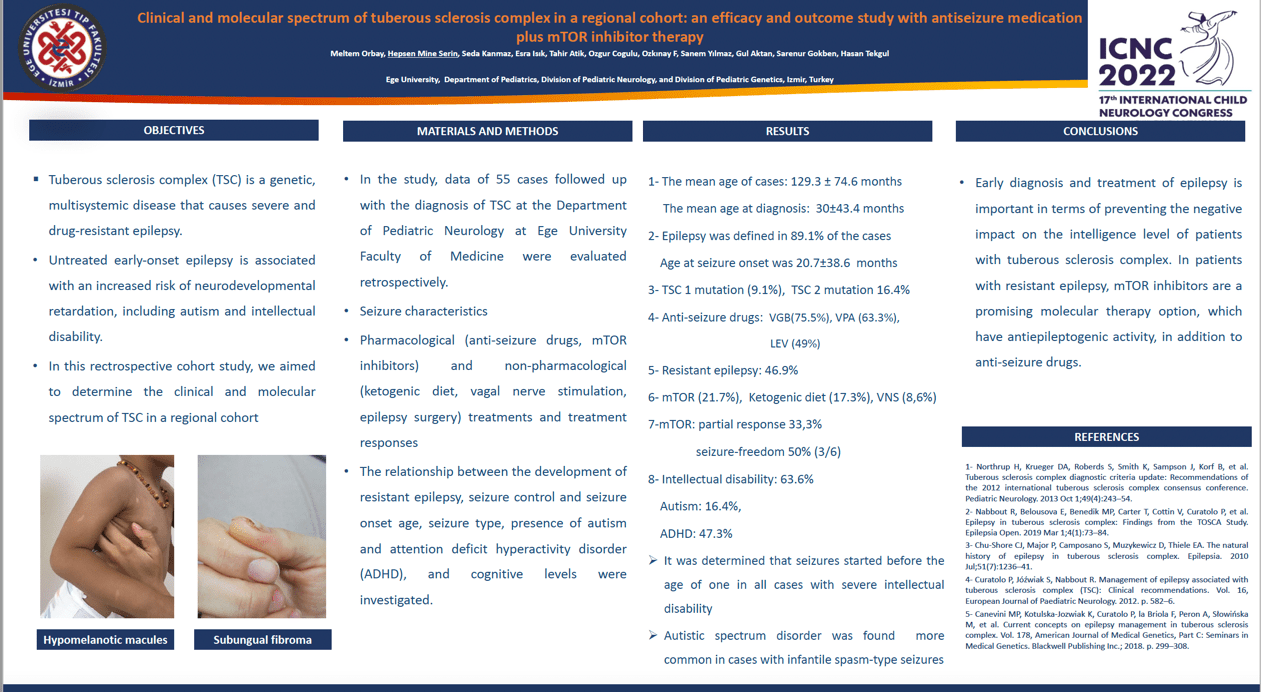
Objective: Tuberous sclerosis complex (TSC) is a genetic, multisystemic disease that causes severe and drug-resistant epilepsy. In this rectrospective cohort study, we aimed to determine the clinical and molecular spectrum of TSC in a regional cohort. Methods: Fifty-five patients who had been followed at least one year follow-up after the initial diagnosis enrolled in the study with using Revised Diagnostic Criteria for Tuberous Sclerosis Complex. Clinical demographics ( seizure semiology, seizure-onset age, antiseizure medication-ASM, mTOR therapy, seizure control rate, drug-refractory epilepsy-DRE, co-morbidities including autism and ADHD, and cognitive levels), EEG characteristics, MRI findings, and molecular spectrum were evaluated. Results: Active epilepsy was defined as 89.1% (n=49) in the study group. Other co-morbities were intellectual disability ( 63.6%), ADHD ( 47.2%) and autism ( 16.3%). Genetic analysis (n=18) revealed a pathogenic mutation (n=14, 78%) in the TSC1 (28%) or TSC2 gene (50%). Active epilepsy was defined with 80% in TSC1 mutation (+) patients and with 88.9% in TSC2 mutation (+) patients. DRE was defined in 47% (n=23) of patients with active epilepsy. Vigabatrin was selected as first ASM in 30% (n=15) of patients with active epilepsy and DRE occurred with 33.3% . Combined therapy (VGB plus mTOR therapy) was performed in 28 (57%) of the cohort with a favorable outcome in 46.2% (n=12). Non-pharmacologic therapy (ketogenic diet and VNS ) was applied in 6 (12.2%) patients with DRE.
Conclusion: A favorable seizure and overall outcome might be obtainable with early antiepileptic treatment of active epilepsy in patients with TSC.
Keywords: Tuberous sclerosis complex; epilepsy; anti-seizure drugs; mTOR inhibitor; intellectual disability
Meltem Orbay
Ege University
Turkey
Hepsen Mine Serin
Ege University
Turkey
Seda Kanmaz
Ege University, Department of Pediatrics, Division of Pediatric Neurology
Turkey
Esra Isik
Ege University
Turkey
Tahir Atik
Ege University
Turkey
Ozgur Cogulu
Ege University
Turkey
Ferda Ozkinay
Ege University
Turkey
Sanem Yılmaz
Ege University
Turkey
Gul Aktan
Ege University
Turkey
Sarenur Gökben
Ege University
Turkey
Hasan Tekgül
Ege University
Objective: Tuberous sclerosis complex (TSC) is a genetic, multisystemic disease that causes severe and drug-resistant epilepsy. In this rectrospective cohort study, we aimed to determine the clinical and molecular spectrum of TSC in a regional cohort. Methods: Fifty-five patients who had been followed at least one year follow-up after the initial diagnosis enrolled in the study with using Revised Diagnostic Criteria for Tuberous Sclerosis Complex. Clinical demographics ( seizure semiology, seizure-onset age, antiseizure medication-ASM, mTOR therapy, seizure control rate, drug-refractory epilepsy-DRE, co-morbidities including autism and ADHD, and cognitive levels), EEG characteristics, MRI findings, and molecular spectrum were evaluated. Results: Active epilepsy was defined as 89.1% (n=49) in the study group. Other co-morbities were intellectual disability ( 63.6%), ADHD ( 47.2%) and autism ( 16.3%). Genetic analysis (n=18) revealed a pathogenic mutation (n=14, 78%) in the TSC1 (28%) or TSC2 gene (50%). Active epilepsy was defined with 80% in TSC1 mutation (+) patients and with 88.9% in TSC2 mutation (+) patients. DRE was defined in 47% (n=23) of patients with active epilepsy. Vigabatrin was selected as first ASM in 30% (n=15) of patients with active epilepsy and DRE occurred with 33.3% . Combined therapy (VGB plus mTOR therapy) was performed in 28 (57%) of the cohort with a favorable outcome in 46.2% (n=12). Non-pharmacologic therapy (ketogenic diet and VNS ) was applied in 6 (12.2%) patients with DRE.
Conclusion: A favorable seizure and overall outcome might be obtainable with early antiepileptic treatment of active epilepsy in patients with TSC.
Keywords: Tuberous sclerosis complex; epilepsy; anti-seizure drugs; mTOR inhibitor; intellectual disability
Meltem Orbay
Ege University
Turkey
Hepsen Mine Serin
Ege University
Turkey
Seda Kanmaz
Ege University, Department of Pediatrics, Division of Pediatric Neurology
Turkey
Esra Isik
Ege University
Turkey
Tahir Atik
Ege University
Turkey
Ozgur Cogulu
Ege University
Turkey
Ferda Ozkinay
Ege University
Turkey
Sanem Yılmaz
Ege University
Turkey
Gul Aktan
Ege University
Turkey
Sarenur Gökben
Ege University
Turkey
Hasan Tekgül
Ege University
Hepsen Mine Serin
Ege University
Turkey
Ege University
Turkey