Reversible Leigh’s-like brain abnormalities with Vigabatrin: A Case Series
Surbhi Gupta, Ramesh Konanki, Nihaal Reddy, Lokesh Lingappa
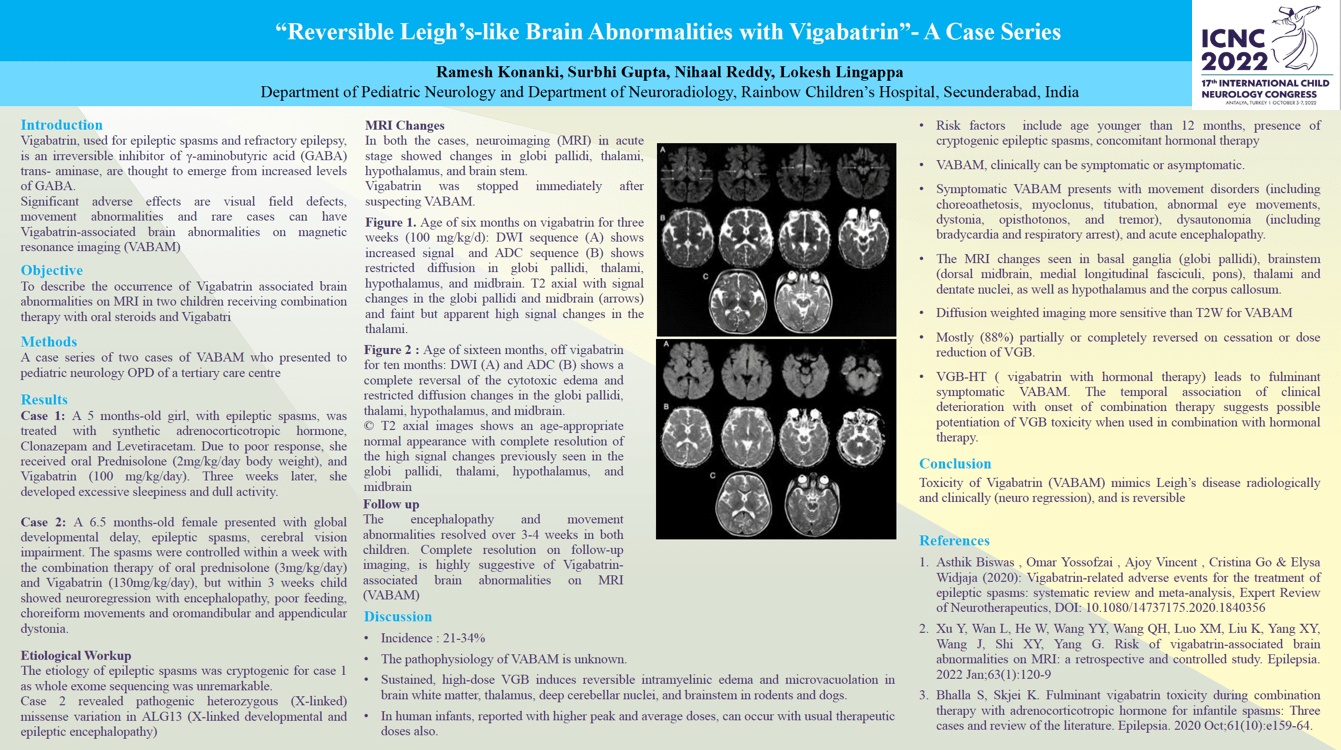
Objectives: To describe the occurrence of Vigabatrin associated brain abnormalities on MRI in two children receiving combination therapy with oral steroids and Vigabatrin Methods: A case series of two cases of VABAM who presented to pediatric neurology OPD of a tertiary care centre. Results: Case 1: A 5 months-old girl, with epileptic spasms, was treated with synthetic adrenocorticotropic hormone, Clonazepam and Levetiracetam. Due to poor response, she received oral Prednisolone (2 mg/kg/day body weight), and Vigabatrin (100 mg/kg/day). Three weeks later, she developed excessive sleepiness and dull activity. Case 2: A 6.5 months-old female presented with global developmental delay, epileptic spasms, cerebral vision impairment. The spasms were controlled within a week with the combination therapy of oral prednisolone (3mg/kg/day) and Vigabatrin (130mg/kg/day), but child showed regression with encephalopathy, poor feeding, choreiform movements and oromandibular and appendicular dystonia. In both children, neuroimaging (MRI) revealed abnormalities involving globi pallidi, thalami, hypothalamus, and brain stem, with complete resolution on follow-up imaging, suggestive of Vigabatrin-associated brain abnormalities on MRI (VABAM) (figure 1). The whole exome sequencing for case 1 was unremarkable and case 2 revealed pathogenic heterozygous (X-linked) missense variation in ALG13 (X-linked developmental and epileptic encephalopathy). The encephalopathy and movement abnormalities resolved over 3-4 weeks in both children upon withdrawal of Vigabatrin, and follow-up MRI (after 2 months) showed resolution of earlier changes (figure 2). Conclusion: The risk of VABAM, through intramyelinic edema, is dose-dependent, and increases with co-hormonal therapy. It mimics mitochondrial cytopathies and metabolic disorders.
Keywords: Vigabatrin, VABAM, Epileptic spasms
Surbhi Gupta
Rainbow Children's Hospital, Hyderabad, India
India
Ramesh Konanki
Rainbow Children's Hospital, Hyderabad, India
India
Nihaal Reddy
Tenet Diagnostics
India
Lokesh Lingappa
Rainbow Children's Hospital, Hyderabad, India
India
Objectives: To describe the occurrence of Vigabatrin associated brain abnormalities on MRI in two children receiving combination therapy with oral steroids and Vigabatrin Methods: A case series of two cases of VABAM who presented to pediatric neurology OPD of a tertiary care centre. Results: Case 1: A 5 months-old girl, with epileptic spasms, was treated with synthetic adrenocorticotropic hormone, Clonazepam and Levetiracetam. Due to poor response, she received oral Prednisolone (2 mg/kg/day body weight), and Vigabatrin (100 mg/kg/day). Three weeks later, she developed excessive sleepiness and dull activity. Case 2: A 6.5 months-old female presented with global developmental delay, epileptic spasms, cerebral vision impairment. The spasms were controlled within a week with the combination therapy of oral prednisolone (3mg/kg/day) and Vigabatrin (130mg/kg/day), but child showed regression with encephalopathy, poor feeding, choreiform movements and oromandibular and appendicular dystonia. In both children, neuroimaging (MRI) revealed abnormalities involving globi pallidi, thalami, hypothalamus, and brain stem, with complete resolution on follow-up imaging, suggestive of Vigabatrin-associated brain abnormalities on MRI (VABAM) (figure 1). The whole exome sequencing for case 1 was unremarkable and case 2 revealed pathogenic heterozygous (X-linked) missense variation in ALG13 (X-linked developmental and epileptic encephalopathy). The encephalopathy and movement abnormalities resolved over 3-4 weeks in both children upon withdrawal of Vigabatrin, and follow-up MRI (after 2 months) showed resolution of earlier changes (figure 2). Conclusion: The risk of VABAM, through intramyelinic edema, is dose-dependent, and increases with co-hormonal therapy. It mimics mitochondrial cytopathies and metabolic disorders.
Keywords: Vigabatrin, VABAM, Epileptic spasms
Surbhi Gupta
Rainbow Children's Hospital, Hyderabad, India
India
Ramesh Konanki
Rainbow Children's Hospital, Hyderabad, India
India
Nihaal Reddy
Tenet Diagnostics
India
Lokesh Lingappa
Rainbow Children's Hospital, Hyderabad, India
India
Surbhi Gupta
Rainbow Children's Hospital, Hyderabad, India India
Rainbow Children's Hospital, Hyderabad, India India