A case of first pediatric pseudotumor cerebri syndrome secondary to superior sagittal sinus thrombosis associated with SARS-CoV-2
Mehmet Can Yeşilmen, Çağatay Günay, Gamze Uzan Sarıkaya, Özlem Özsoy, Semra Hız Kurul, Elif Yaşar, Uluç Yiş
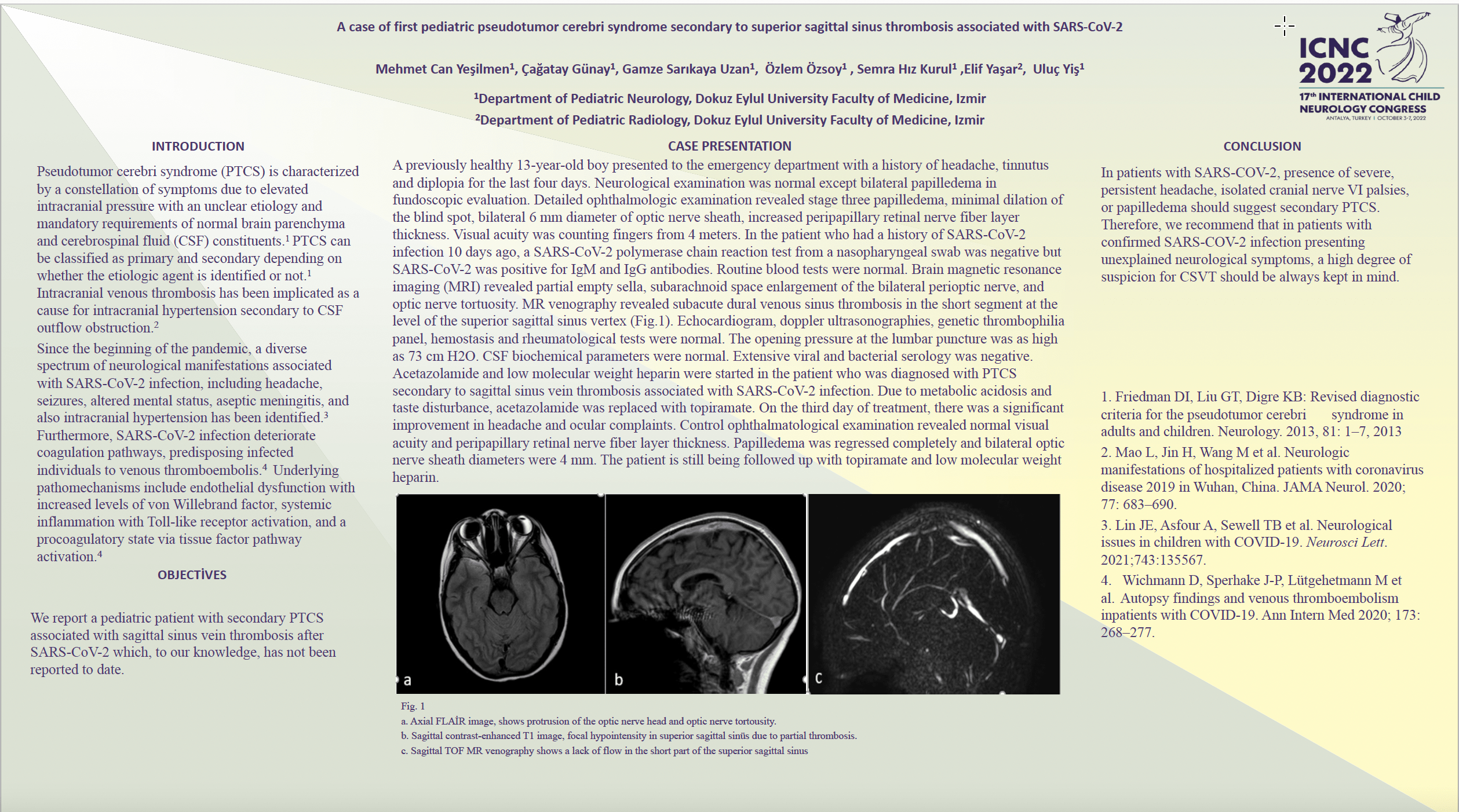
Introduction: Pseudotumor cerebri syndrome (PTCS) is defined as the presence of elevated intracranial pressure in the environment of normal brain parenchyma and cerebrospinal fluid. PTCS can occur in pediatric populations and can cause permanent vision loss if left untreated. It is known that SARS-CoV-2 infection predisposes patients to arterial and venous thromboembolic events. Several reports from the literature suggest that cerebral venous sinus thrombosis (CVST) may be a direct complication of SARS-CoV-2. We aimed to report a case of PTCS secondary to superior sagittal sinus thrombosis associated with the first pediatric SARS-CoV-2 infection. Case: A previously healthy 13-year-old boy presented with a 4-day history of headache, tinnutus and diplopia. His mental status and cranial nerve examination were normal in his neurological examination at admission, bilateral papilledema was detected in fundus examination. SARS-CoV-2 polymerase chain reaction was negative, while anti-SARS-CoV-2 antibody was positive. Contrast-enhanced brain magnetic resonance imaging showed signs of intracranial hypertension and MR venography showed superior sagittal sinus thrombosis. The lumbar puncture showed high opening pressure (73cmH2O). He was treated with low molecular weight heparin, topiramate. Our patient was diagnosed as PTS secondary to CVST associated with SARS-CoV-2 infection. Conclusion: PTCS secondary to CVST associated with SARS-CoV-2 infection was diagnosed and the child was treated with oral topiramate, low molecular weight heparin. After treatment, headache, visual functions improved and the child was followed up. Clinicians should consider the risk of acute CVST in SARS-CoV-2 positive patients, especially if neurological symptoms develop. Early diagnosis and treatment can prevent vision loss.
Keywords: SARS-CoV-2, Pseudotumor cerebri, papilledema, cerebral venous sinus thrombosis, CVST
Mehmet Can Yeşilmen
Dokuz Eylul University Faculty of Medicine
Turkey
Çağatay Günay
Dokuz Eylul University Faculty of Medicine
Turkey
Gamze Uzan Sarıkaya
Dokuz Eylul University Faculty of Medicine
Turkey
Özlem Özsoy
Dokuz Eylul University Faculty of Medicine
Turkey
Semra Hız Kurul
Dokuz Eylul University Faculty of Medicine
Turkey
Elif Yaşar
Dokuz Eylul University Faculty of Medicine
Turkey
Uluç Yiş
Dokuz Eylul University Faculty of Medicine
Turkey
Introduction: Pseudotumor cerebri syndrome (PTCS) is defined as the presence of elevated intracranial pressure in the environment of normal brain parenchyma and cerebrospinal fluid. PTCS can occur in pediatric populations and can cause permanent vision loss if left untreated. It is known that SARS-CoV-2 infection predisposes patients to arterial and venous thromboembolic events. Several reports from the literature suggest that cerebral venous sinus thrombosis (CVST) may be a direct complication of SARS-CoV-2. We aimed to report a case of PTCS secondary to superior sagittal sinus thrombosis associated with the first pediatric SARS-CoV-2 infection. Case: A previously healthy 13-year-old boy presented with a 4-day history of headache, tinnutus and diplopia. His mental status and cranial nerve examination were normal in his neurological examination at admission, bilateral papilledema was detected in fundus examination. SARS-CoV-2 polymerase chain reaction was negative, while anti-SARS-CoV-2 antibody was positive. Contrast-enhanced brain magnetic resonance imaging showed signs of intracranial hypertension and MR venography showed superior sagittal sinus thrombosis. The lumbar puncture showed high opening pressure (73cmH2O). He was treated with low molecular weight heparin, topiramate. Our patient was diagnosed as PTS secondary to CVST associated with SARS-CoV-2 infection. Conclusion: PTCS secondary to CVST associated with SARS-CoV-2 infection was diagnosed and the child was treated with oral topiramate, low molecular weight heparin. After treatment, headache, visual functions improved and the child was followed up. Clinicians should consider the risk of acute CVST in SARS-CoV-2 positive patients, especially if neurological symptoms develop. Early diagnosis and treatment can prevent vision loss.
Keywords: SARS-CoV-2, Pseudotumor cerebri, papilledema, cerebral venous sinus thrombosis, CVST
Mehmet Can Yeşilmen
Dokuz Eylul University Faculty of Medicine
Turkey
Çağatay Günay
Dokuz Eylul University Faculty of Medicine
Turkey
Gamze Uzan Sarıkaya
Dokuz Eylul University Faculty of Medicine
Turkey
Özlem Özsoy
Dokuz Eylul University Faculty of Medicine
Turkey
Semra Hız Kurul
Dokuz Eylul University Faculty of Medicine
Turkey
Elif Yaşar
Dokuz Eylul University Faculty of Medicine
Turkey
Uluç Yiş
Dokuz Eylul University Faculty of Medicine
Turkey
Mehmet Can Yeşilmen
Dokuz Eylul University Faculty of Medicine
Turkey
Dokuz Eylul University Faculty of Medicine
Turkey