Gelastic Seizures Beyond Hypothalamic Hamartomas - Prevalence And Outcome
GELASTIC SEIZURES BEYOND HYPOTHALAMIC HAMARTOMAS PREVALENCE AND OUTCOME Dr. Manisha Karamala Yalapalli, Dr. Ramshekhar N Menon, Dr. Ashalatha Radhakrishnan R. Madhavan Nair Center for Comprehensive Epilepsy Care, Sree Chitra Tirunal Institute for Medical Sciences and Technology.
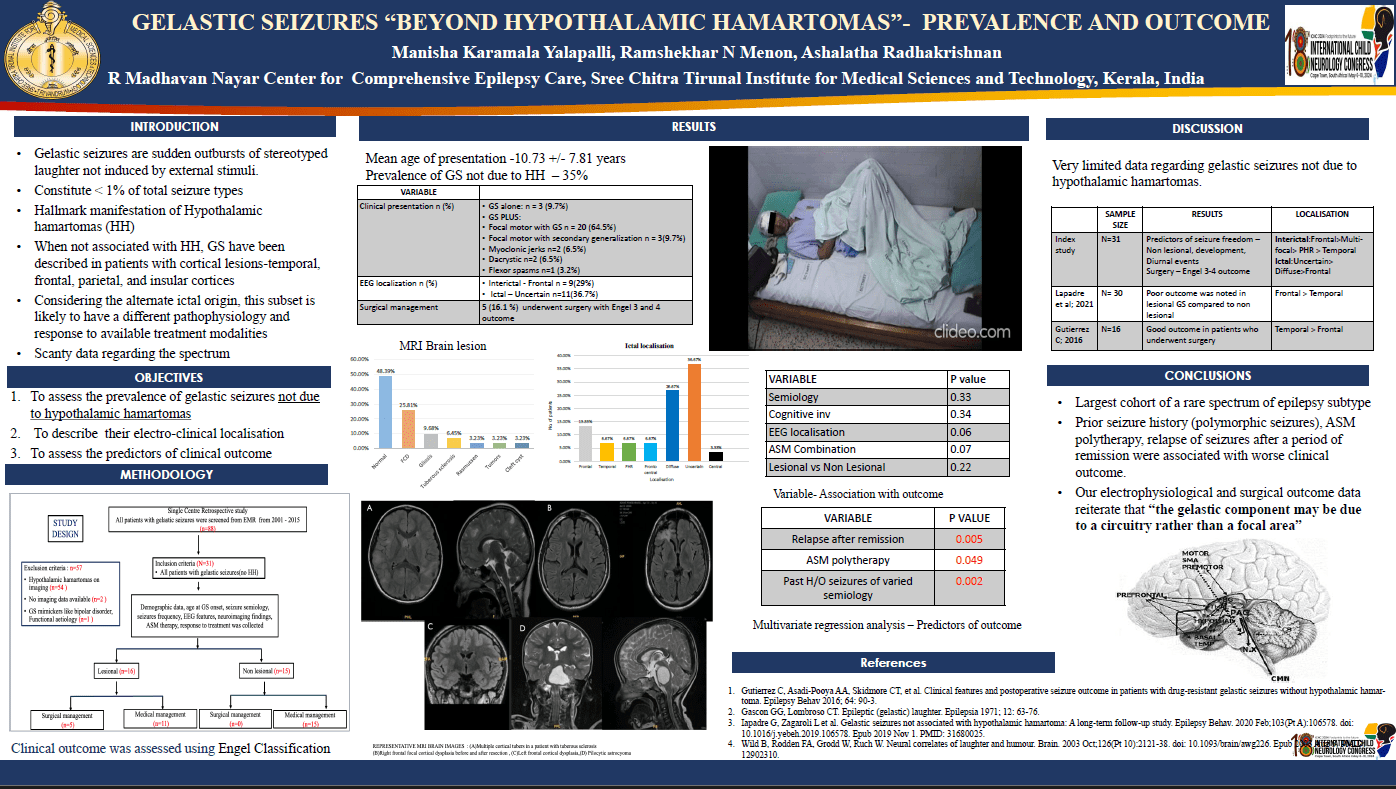
Aims: Gelastic seizures (GS) constitute <1% prevalence of which those due to non-hypothalamic hamartomas (HH) are rarer. There is scanty data regarding the spectrum. We aimed to assess prevalence of GS due to non HH, electroclinical (EC) localization and predictors of outcome.
Methods: Single center retrospective study where patients with gelastic seizures with etiology beyond HH from 2001 to 2015 were included. The electroclinical data of the patients was collected from electronic medical records. Predictors of short term (6 months) and long term(5yrs) outcome were analyzed.
Results: Among total patients of GS (n=88), etiologies other than HH were identified in 35.22% (n=31) with mean age of onset 6.29 ±6.12 years. Most common electroclinical localization was frontal and posterior head region. Structural lesion was noted in 51.6% of patients, most common being focal cortical dysplasia followed by gliosis, tuberous sclerosis, Rasmussen’s encephalitis.16% of patients underwent surgical treatment. Predictors of worse outcome were polytherapy (p=0.04), surgery (p=0.007), post remission relapse (p=0.005), prior history of seizures (p=0.002). Structural lesion, semiology, EC localization did not affect outcome.
Conclusion: Prevalence of non HH etiologies among GS is 35%. Patients with prior history of seizures of varied semiology, underwent surgery, on polytherapy and those who relapsed after a period of remission were associated with worse outcome.
I have no disclosures.
Manisha Karamala Yalapalli
SCTIMST
India
Ramshekhar N Menon
SCTIMST
India
Ashalatha Radhakrishnan
SCTIMST
India