Management And Treatment Choices In Pediatric Rasmussen’s Encephalitis: A Single Center Case Series.
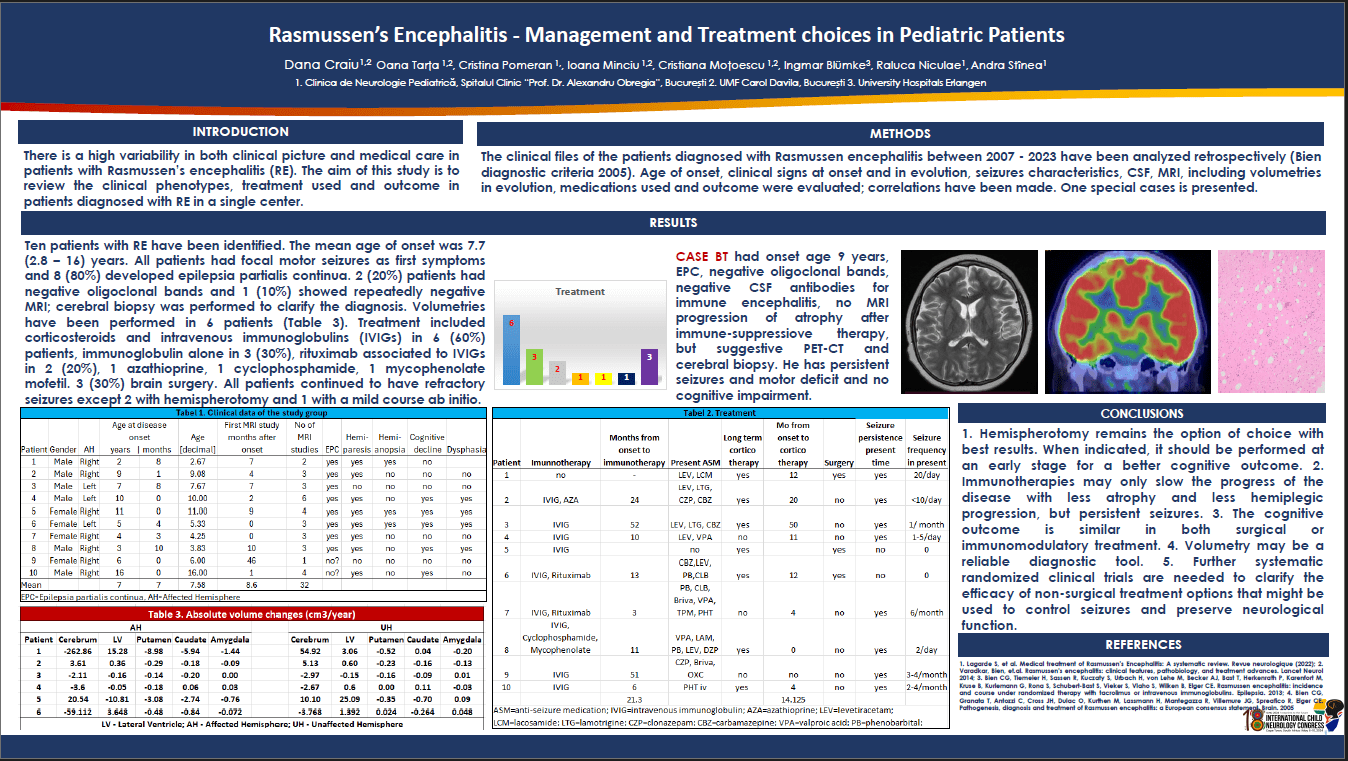
INTRODUCTION: The aim of this study is to review the clinical phenotypes, treatments used and outcome in patients diagnosed with Rasmussen’s encephalitis (RE). METHODS: A retrospective study analyzed the clinical files of the patients diagnosed between 2007 - 2023 with Rasmussen encephalitis (Bien diagnostic criteria 2005). Age of onset, clinical signs at onset and in evolution, seizures characteristics, CSF, MRI, including volumetries in evolution, medications used and outcome were evaluated; correlations have been made. RESULTS: Ten patients with RE have been identified. The mean age of onset was 7.7 (2.8 – 16) years. All patiens had focal motor seizures as first symptoms and 8 (80%) developed epilepsia partialis continua. 2 (20%) patients had negative oligoclonal bands and 1 (10%) showed repeatedly negative MRI; cerebral biopsy was performed to clarify the diagnosis. Treatment included corticosteroids and intravenous immunoglobulins (IVIGs) in 4 (40%) patients, immunoglobulin alone in 5 (50%), rituximab associated to IVIGs in 2 (20%), 1 received azathioprine, 1 cyclophosphamide, 1 mycophenolate mofetil. 3 (30%) underwent brain surgery. At the latest follow-up, all patients continued to have refractory seizures except for 2 patients who underwent hemispherotomy and 1 with a mild course ab initio. CONCLUSION: Hemispherotomy remains the treatment option of choice for management of seizures in RE preventing repeated hospitalization and insuring seizure and medication freedom. The cognitive and neurological outcome are similar in both surgical or immunomodulatory treatment. Selected special cases (1 MRI negative, 1 with spontaneous good outcome) are presented. DISCLOSURES: nothing to disclose.
Dana Craiu
Carol Davila University of Medicine, Department of Neurosciences, Discipline of Pediatric Neurology
Romania
Oana Tarta-Arsene
Carol Davila University of Medicine, Department of Neurosciences, Discipline of Pediatric Neurology
Romania
Cristina Pomeran
Romania
Ioana Minciu
Carol Davila University of Medicine, Department of Neurosciences, Discipline of Pediatric Neurology
Romania
Cristina Motoescu
Carol Davila University of Medicine, Department of Neurosciences, Discipline of Pediatric Neurology
Romania
Ingmar Blümke
Germany
Raluca Niculae
Carol Davila University of Medicine, Department of Neurosciences, Discipline of Pediatric Neurology
Romania
Andra Stȋnea
Carol Davila University of Medicine, Department of Neurosciences, Discipline of Pediatric Neurology
Romania
Dana Craiu
Carol Davila University of Medicine, Department of Neurosciences, Discipline of Pediatric Neurology
Romania