Skull Infarction In Patients With Sickle Cell Disease
Objective: Osteonecrosis is a well-described complication of sickle cell disease (SCD) that occurs secondary to vaso-occlusion. Skull infarction is rare and presents with unique clinical challenges and complex anatomy involving vital structures that can be life-threatening. This study aims to explore the main clinical and imaging findings in patients with SCD who developed skull infarction.
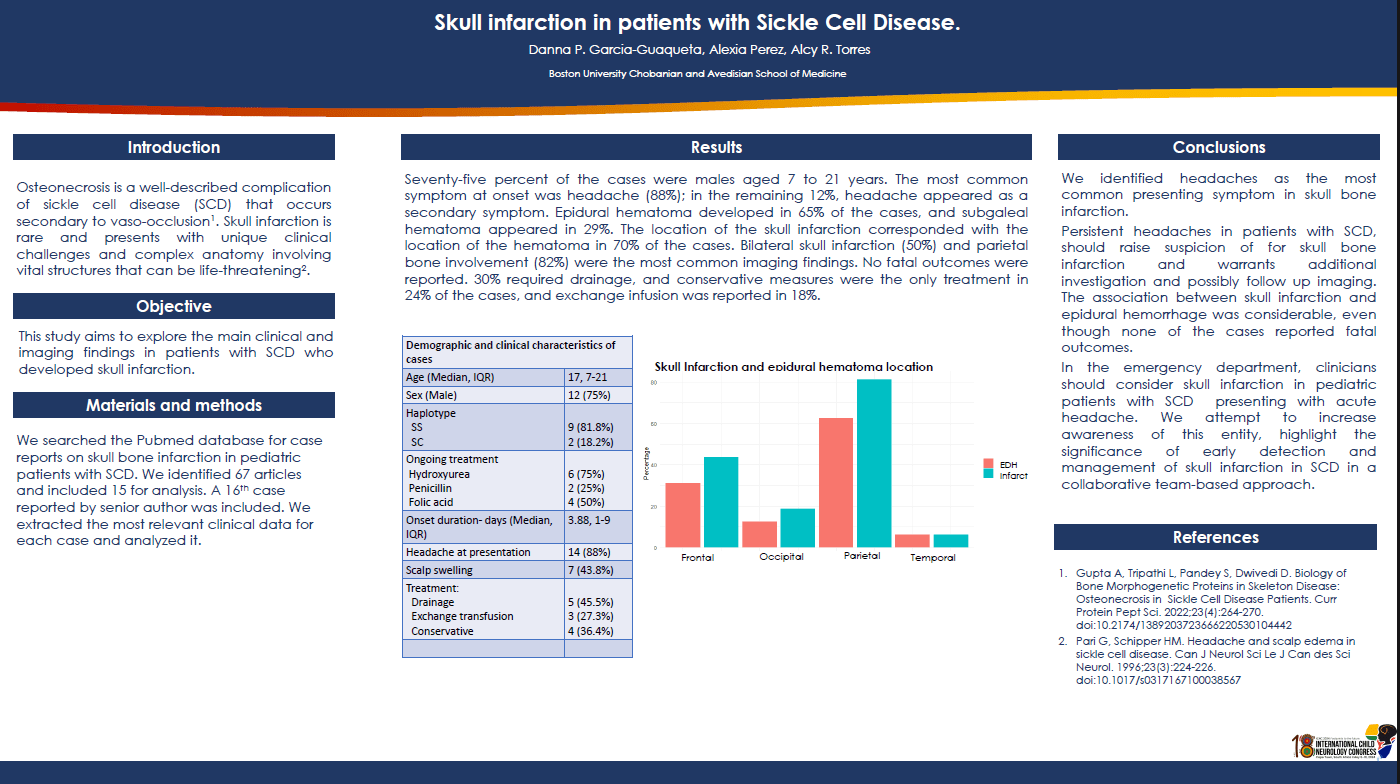
Methods: We searched the Pubmed database for previous reports on skull bone infarction in patients with SCD. We identified 66 articles and included 16 for analysis. We included an additional case who was seen by the senior author. We extracted the most relevant clinical data for each case and analyzed it.
Results: Seventy-six percent of the cases were males aged 7 to 25 years. The most common symptom at onset was headache (88%); in the remaining 12%, headache appeared as a secondary symptom. Epidural hematoma developed in 65% of the cases, and subgaleal hematoma appeared in 29%. The location of the skull infarction corresponded with the location of the hematoma in 70% of the cases. Bilateral skull infarction (52%) and parietal bone involvement (82%) were the most common imaging findings. No fatal outcomes were reported. 30% required drainage, and conservative measures were the only treatment in 24% of the cases, and exchange infusion was reported in 18%.
Conclusions: Although uncommon, skull infarction is a potentially serious comorbidity in patients with SCD. Our study highlights early detection, precise diagnosis, and collaborative care while highlighting the clinical challenges of detecting skull infarction in SCD.
Danna P. Garcia-Guaqueta
M.D., Pediatric Neurology
Boston University Chobanian and Advesian School
Boston, United States
Alexia M. Perez
M.D., Pediatric Neurology
Boston University Chobanian and Advesian School
Boston, United States
Alcy R. Torrez
M.D., Pediatric Neurology
Boston University Chobanian and Advesian School
Boston, United States