Cost Reduction for Families and Healthcare System with the Implementation of a Paediatric Comprehensive Epilepsy Clinic
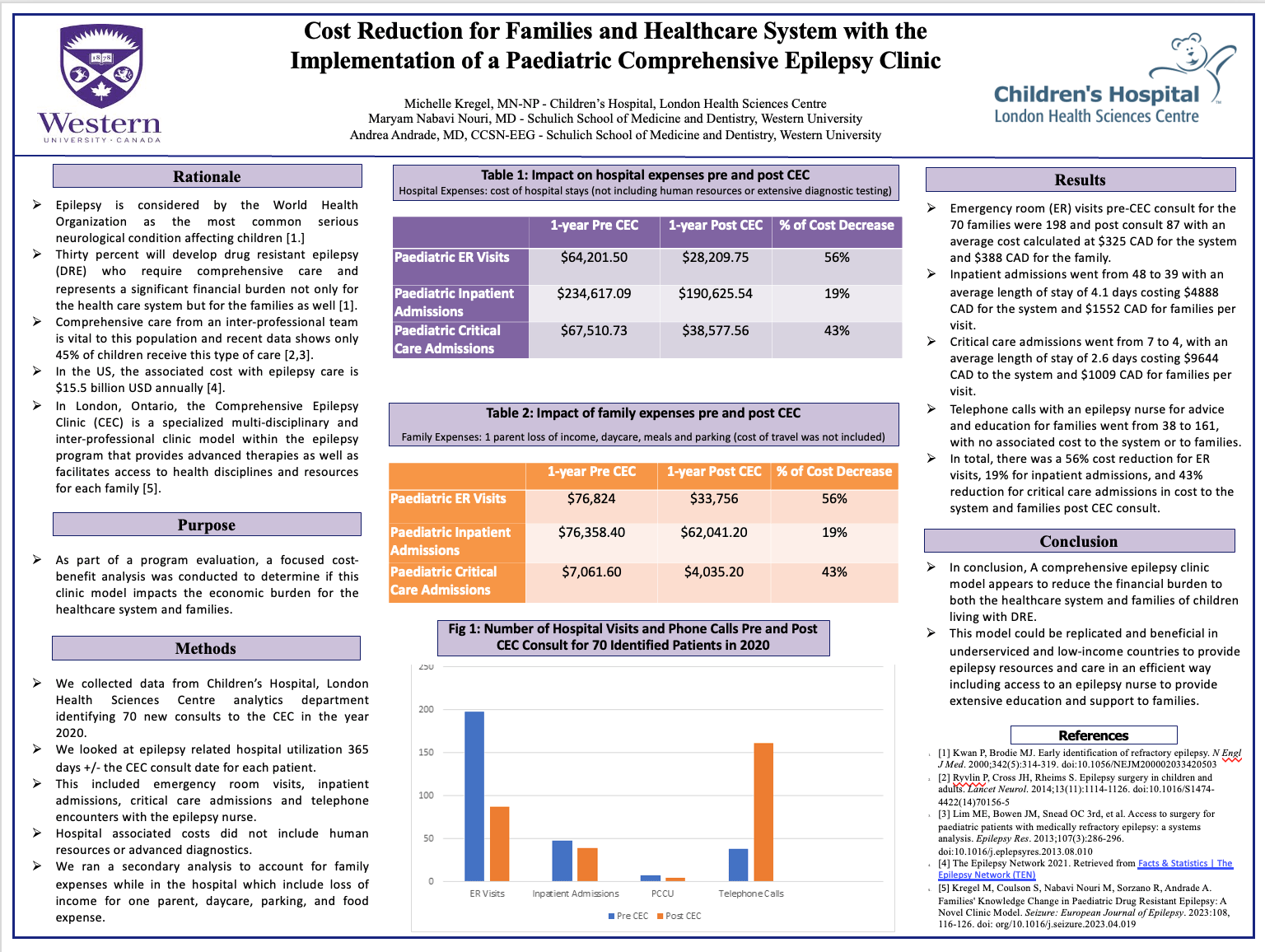
Epilepsy is considered by the WHO as the most common serious neurological condition affecting children. 30% will develop drug resistant epilepsy (DRE) who require comprehensive care and represent a significant financial burden for the health care system and the families. In London, Ontario, the Comprehensive Epilepsy Clinic (CEC) is a specialized multi-disciplinary clinic model that provides advanced therapies and facilitates access to health disciplines and resources. A focused cost-benefit analysis was conducted to determine if this clinic model impacts the economic burden for the healthcare system and families. We collected data identifying 70 new consults to the CEC in the year 2020. We looked at epilepsy related hospital utilization 365 days +/- the CEC consult date for each. This included emergency room (ER) visits, inpatient and critical care admissions and telephone encounters with the epilepsy nurse. ER visits pre-CEC consult went from 198 to 87 post with a 56% cost reduction (CR), inpatient admissions went from 48 to 39 with a 19% CR, critical care admissions went from 7 to 4 with a 43% CR and telephone calls with a nurse for education went from 38 to 161, which has no associated cost to the system or to families. A CEC model appears to reduce the financial burden to both the healthcare system and families of children living with DRE. This model could be replicated and beneficial in underserviced and low-income countries to provide epilepsy care in an efficient way.
Michelle Kregel
Children's Hospital, London Health Sciences Centre
Canada
Maryam Nabavi Nouri
Schulich School of Medicine & Dentistry
Canada
Andrea Andrade
Schulich School of Medicine & Dentistry
Canada